
by All Things Neonatal | Jan 28, 2016 | marijuana
Gastroschisis, a condition in which the bowel herniates out of the abdomen during fetal development, is on the rise. The rising incidence which occurs about 2000 times a year in the US caught the interest of CNN in a piece on their site this week. Canada is no different with rates seeming to increase steadily over the last decade or so and many of us who care for these infants are left scratching our heads as to why.
What Causes Gastroschisis to Occur
Interestingly, the site of herniation is almost always to the right of the umbilicus and the most prevalent theory out there is that a vascular insult during fetal development leads to a weakening in the developing abdominal wall. The bowel then herniates through this insufficiency. What then could could explain the near universal occurence on the right? The Vascular Disruption Theory.
You may not have known this but the embryo begins life with two umbilical veins and two omphalomesenteric arteries. At about one month of gestation the right umbilical vein involutes leaving you with only one umbilical vein. In this disruption theory, the vein involution occurs early leading to ischemia in the territory that eventually causes weakness in the abdominal wall to the right of the umbilicus. On the arterial side the left omphalomesenteric artery also involutes, with the right one becoming the superior mesenteric artery. It could be that disruption of this process also leads to gastroschisis.
Risk Factors For Gastroschisis
If you work in the field of Neonatology one of the first surgical truisms you learn in that gastroschisis occurs most commonly among very young mothers. Broadly speaking, gastroschisis also tends to cluster among women of low socioeconomic status (SES) and all that goes with that designation. Poor diet, education and drug use are intimately linked with the condition but in the end the proxy may be low SES. When it comes to drug use it is the drugs that have vasoactive properties that are most often associated with heightened risk for the condition. Such drugs include, amphetamines, cocaine, as well as ibuprofen, acetaminophen. Finally, smoking likely secondary to nicotine and other vasoactive chemicals which may affect placental circulation also finds itself closely linked with development of the condition.
In terms of quantifying the risk, Draper et al performed a case control study to quantify the risk of such use. The interesting aspect of their study is that they confirmed drug use through analysis of maternal hair to demonstrate exposure. Previous studies relied on maternal interviews to disclose which drugs had been used in pregnancy which may be prone to omission. They found the following
1) Any recreational drug – odds ratio (OR) 2.2, 95% confidence interval (CI): 1.2, 4.3)
2) Vasoconstrictive recreational drugs (cocaine, amphetamines & ecstasy) (OR 3.3, 95% CI: 1.0, 10.5)
3) Aspirin use (OR 20.4, 95% CI: 2.2, 191.5)
4) Cigarette smoking (OR 1.7, 95% CI: 1.1, 2.6)
So drugs from a variety of classes seem to increase risk for the condition. Could a rise in drug use in young women account for the increase then?
Trends in Drug Use
The National Institute of Drug Abuse provides some interesting data in this regard. The following curve demonstrates the trend in drug use in the US over a period that has seen the incidence of gastroschisis rise almost two fold. The data collected on this site is obtained from surveys and as such is prone to the same errors that any survey has namely how sure are we that what is disclosed is the reality? Having said that it is clear that in terms of illicit drug use, cannabis accounts for the majority of the rise in use over the last decade.
Furthermore, it is well known that cannabis is a “gateway drug” and the same site indicates that over 50% of new users are under the age of 18 and of these new users the drug of choice is marijuana.
Looking at pain relievers such as tylenol and ibuprofen there is no data to suggest at least in the very young group of mothers consumption of these medications has been on the rise. Clearly we have a problem with over prescription of opioid analgesics in pregnancy but to my knowledge these have not been associated with the development of gastroschisis.
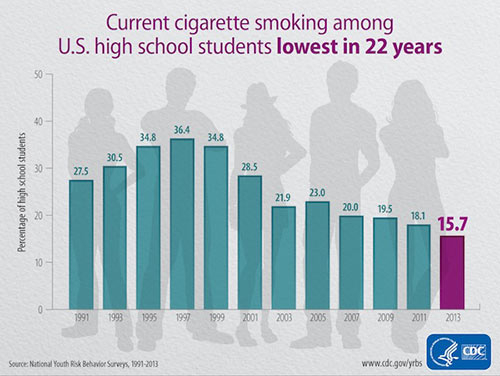
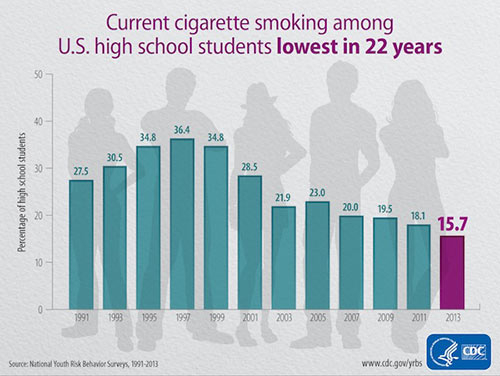
What about smoking in teens?
As the graph from the CDC below demonstrates, smoking is at an all time low among US high school students. These same students are the ones having babies with gastroschisis so at first glance this doesn’t seem to be a probable cause. Are rates among low SES students showing the same decline? A shown in this link, rates even among these groups do seem to be declining as well even though level of education does show correlations with higher prevalence of smokers.
Could Increased Cannabis Use Be The Culprit?
Almost twenty years ago a surgeon mentioned to me on a rotation during my residency that he had noted an association between marijuana use and gastroschisis.  While I don’t believe this was ever published I have to admit it stuck as if it were gospel. Some years later in another conversation about a patient with gastroschisis he said with a smile that after all these years he believes the link is an association. Young mothers use more marijuana and they also have more babies with gastroschisis. What we have here now though is something a little different. The question at hand is why is gastroschisis on the rise in the same group?
While I don’t believe this was ever published I have to admit it stuck as if it were gospel. Some years later in another conversation about a patient with gastroschisis he said with a smile that after all these years he believes the link is an association. Young mothers use more marijuana and they also have more babies with gastroschisis. What we have here now though is something a little different. The question at hand is why is gastroschisis on the rise in the same group?
Is it cannabis? It just might be but this will need some further work to tease out. If gastroschisis is caused by a vascular phenomenon and the only real rise in drug use affecting perfusion is that associated with cannabis, it might be. On the other hand this could just be another association that will not stand the test of time. I don’t have it in for cannabis and in fact believe it could one day be quite useful in Neonatology as I have written before in Marijuana Coming Soon To An NICU Near You!
What goes around comes around as the saying goes and as my colleague nears the end of his long and storied career that in the end his original observation would be proven true. I have no wish for cannabis to be linked to the increase in gastroschisis but a part of me would love to see my colleague proven right after all these years. Stay tuned!

by All Things Neonatal | Jan 7, 2016 | Innovation, Neonatology, Prematurity
In the spirit of full disclosure I have to admit I have never placed a laryngeal mask airway (LMA) in a newborn of any gestational age. I have played with them in simulated environments and on many occasion mentioned that they are a great alternative to an ETT especially in those situations where intubation may not be possible due to the skill of the provider or the difficulty of the airway in the setting of micrognathia for example.
In recent years though we have heard of examples of surfactant delivery via these same devices although typically these were only case reports. More recently a small randomized study of 26 infants by Attridge et al demonstrated in the group randomized to surfactant administration through an LMA that oxygen requirements were reduced after dosing. This small pilot provides sufficient evidence to show that it is possible to provide surfactant and that at least some gets into the airway of the newborn. This proof of concept though while interesting, did not answer the question of whether such delivery of surfactant would be the same or better than through an ETT. As readers of my blog posts know, my usual stance on things is that the less invasive the better and as I look through the literature, I am drawn to concepts such as this to see if they can be added to our toolbox of non or less invasive strategies in the newborn.
A Minimally Invasive Technique For The Masses?
This past month, a small study by Pinheiro et al sought to answer this question by using 61 newborns between 29 0/7 – 36 6/7 weeks and greater than 1000g and randomizing them to either surfactant via the INSURE technique or LMA. I cannot stress enough so will get it out of the way at the start that this strategy is not for those <1000g as the LMA is not designed to fit them properly and the results (to be shown) should not be generalized to this population. Furthermore then study included only those infants who needed surfactant between 4 – 48 hours of age, were on CPAP of at least 5 cm H2O and were receiving FiO2 between 30 – 60%. All infants given surfactant via the insure technique were premedicated with atropine and morphine while those having an LMA received atropine only. The primary outcome of the study was need for subsequent intubation or naloxone within 1 hour of surfactant administration. The study was stopped early after an interim analysis (done as the fellow involved was finishing their fellowship – on a side note I find this an odd reason to stop) demonstrated better outcomes in the group randomized to the LMA.
Before we get into the results let’s address the possible shortcomings of the study as they might already be bouncing around your heads. This study could not be blinded and therefore there could be a significant bias to the results. The authors did have predetermined criteria for reintubation and although not presented, indicate that those participating stuck to these criteria so we may have to acknowledge they did the best they could here. Secondly the study did not reach their numbers for enrolment based on their power calculation. This may be ok though as they found a difference which is significant. If they had found no difference I don’t think I would be even writing this entry! Lastly this study used a dose of surfactant at 3 mL/kg. How well would this work with the formulation that we use BLES that requires 5 mL/kg?
What were the results?
| Intervention Failure |
LMA Group |
ETT group |
p |
| Any failure |
9 (30%) |
23(77%) |
<0.001 |
| Early failure |
1 (3%) |
20 (67%) |
<0.001 |
| Late failure |
8 (27%) |
3 (10%) |
0.181 |
What do these results tell us? The majority of failures occurred within an hour of delivery of surfactant in the ETT group? How does this make any sense? Gastric aspirates for those in the LMA group but not the INSURE group suggest some surfactant missed the lung in the former so one would think the intubation group should have received more surfactant overall however it would appear to be the premedication. The rate of needing surfactant afterwards is no different and in fact there is a trend to needing reintubation more often in the LMA group but the study was likely underpowered to detect this difference. Only two patients were given naloxone to reverse the respiratory depressive effects of morphine in those given the INSURE technique so I can’t help but speculate that if this practice was more frequent many of the reintubations might have been avoided. This group was quite aggressive in sticking to the concept of INSURE as they aimed to extubate following surfactant after 5 – 15 minutes. I am a strong advocate of providing RSI to those being electively intubated but if the goal is to extubate quickly then I believe one must be ready to administer naloxone soon after extubation if signs of respiratory depression are present and this did not happen effectively in this study. Some may argue those getting the INSURE technique should not be given any premedication at all but that is a debate that will go on for years I am sure but they may have a valid point given this data.
Importantly complications following either procedure were minimal and no different in either group.
Where do we go from here?
Despite some of the points above I think this study could prove to be important for several reasons. I think it demonstrates that in larger preterm infants it is possible to avoid any mechanical ventilation and still administer surfactant. Many studies using the minimally invasive surfactant treatment (MIST) approach have been done but these still require the skill of laryngoscopy which takes a fair bit of skill to master. The LMA on the other hand is quite easy to place and is a skill that can be taught widely. Secondly, we know that even a brief period of over distension from PPV can be harmful to the lung therefore a strategy which avoids intubation and direct pressure to the lung may offer some longer term benefit although again this was not the study to demonstrate that.
Lastly, I see this as a strategy to look at in more rural locations where access to highly skilled level III care may not be readily available. We routinely field calls from rural sites with preterm infants born with RDS and the health care provider either is unable to intubate or is reluctant to try in favour of using high flow oxygen via mask. Many do not have CPAP either to support such infants so by the time our Neonatal Transport team arrives the RDS is quite significant. Why not try surfactant through the LMA? If it is poorly seated over the airway and the dose goes into the stomach I don’t see them being in any worse shape than if they waited for the team to arrive. If some or all of the dose gets in though there could be real benefit.
Might this be right for your centre? As we think about outreach education and NRP I think this may well become a strong reason to spend a little more time on LMA training. We may be on to something!

 While I don’t believe this was ever published I have to admit it stuck as if it were gospel. Some years later in another conversation about a patient with gastroschisis he said with a smile that after all these years he believes the link is an association. Young mothers use more marijuana and they also have more babies with gastroschisis. What we have here now though is something a little different. The question at hand is why is gastroschisis on the rise in the same group?
While I don’t believe this was ever published I have to admit it stuck as if it were gospel. Some years later in another conversation about a patient with gastroschisis he said with a smile that after all these years he believes the link is an association. Young mothers use more marijuana and they also have more babies with gastroschisis. What we have here now though is something a little different. The question at hand is why is gastroschisis on the rise in the same group?
