
by All Things Neonatal | May 26, 2016 | Uncategorized
We have been seemingly under siege over the last year or so by a relentless flow of preterm infants through our units in the city. Peaks and valleys for patient census come and go for the most part but this almost unwavering tendency to be filled to the rafters so to speak is unusual. Much has been said and will continue to be acknowledged that we are all doing incredible work, that we are dedicated and putting patients first but where is the breaking point? When does fatigue lead to errors no matter how well intentioned and selfless we are. In those cases when it is not a matter of being selfless but we are mandated to come in fatigue is no less an issue.
Like many units in North America and in other parts of the world, rates of neonatal sepsis have been on the decline but during a recent peak in both acuity and volume in the region we saw a spike in the rate of culture proven sepsis. At a time when we were at our busiest our sepsis rate worsened which raised many eyebrows as to what could be contributing. It is tempting to blame it on patient volumes but what is the actual evidence to support such a claim. This is the thrust of this piece and I hope you find the topic of some relevance to you as we continue on this journey of a higher state of patient volumes in the city.
Nurse to Patient Ratio is Likely Important
This has to be important right?! NICUs come in many shapes and sizes but if you can staff appropriately with 1:1, 1:2 and 1:3 ratios based on patient acuity if you had enough nurses would your sepsis rates be ok? To answer this a useful study is by Jeannie P. Cimiott et al entitled Impact of staffing on bloodstream infections in the neonatal intensive care unit. The study group was actually from an RCT on hand hygiene and this study was a reanalysis of the data to determine for infants with confirmed sepsis what impact nursing hours had in the context of a patient with their first positive blood culture. In her study there were 2675 infants in two New York level III NICUs that had 224 positive blood cultures. The impact of nursing hours on risk of infection was dramatic.
The NICU with greater nursing coverage had a significantly decreased risk (HR, 0.21; 95% CI, 0.06-0.79) of bloodstream infection. Moreover, the more RN hours per nursing intensity weight was associated with a 79% reduction in the risk of bloodstream infection in the unit with greater nursing work hours. 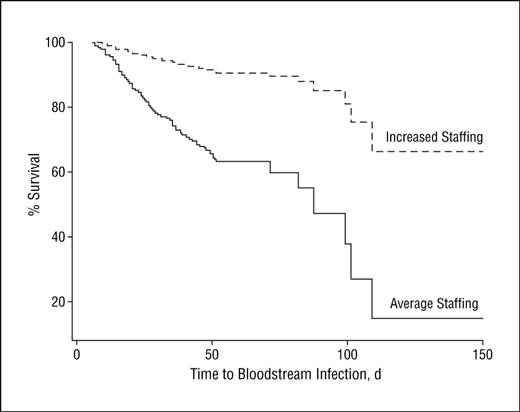 Looking also at the impact of greater nursing hours on time to infection demonstrated the following curve. From the graph one can see that two patients both of which develop an infection at 100 days of life have markedly different chances of survival based on the staffing level. The Neonatologist, RRT, dietician could all be the same but if the nursing hours are lacking the patient is more likely to die. A very significant concern indeed!
Looking also at the impact of greater nursing hours on time to infection demonstrated the following curve. From the graph one can see that two patients both of which develop an infection at 100 days of life have markedly different chances of survival based on the staffing level. The Neonatologist, RRT, dietician could all be the same but if the nursing hours are lacking the patient is more likely to die. A very significant concern indeed!
What Effect Does The Percentage of Preterm Babies In The Unit Have On The Rate of Infections?
The next question may be answered by looking at a study from this year by Goldstein et al entitled Characteristics of late-onset sepsis in the NICU: does occupancy impact risk of infection? This study looked retrospectively at a 17 year period between 1997 and 2014 to determine the risk of systemic infection from two standpoints; occupancy and percentage of infants < 32 weeks. In other words they were looking at whether the presence of many smaller babies in the units increases such risk of infection specifically. This was a rather large study population of 19810 infants of which 446 had confirmed late onset sepsis. Not surprisingly 70% of the cases of sepsis were with CONS.
The authors examined hazard ratios to determine whether occupancy or proportion of infants < 32 weeks had an effect on risk and determined that the average occupancy did not correlate with risk of infection but did for the category of infants < 32 weeks. Interestingly the HR for this was 1.03 with a CI that touches 1 so I am not sure how they make this claim but in the end they conclude:
“For each additional percentage of infants <32 weeks gestation in the unit, neonates had an increased late-onset sepsis hazard of 2% (HR 1.02, 95% CI: 1.00, 1.03) over their NICU hospitalization.”
For arguments sake let’s say this is a real effect. I do have to call into question the diagnosis of sepsis. I could not find mention of the definition of sepsis in this cohort and with so many CONS infections I do worry that some of these were in fact contaminants. Did they draw one or two blood cultures in each instance? How many of these if they had would have had one positive and the other negative? Having just a few of these labelled as contaminants may have negated any effect seen.
What About The Nurses?
You also can’t ignore the fact that while they looked at occupancy they made no attempt to control for the amount of staff. To not do so I think misses a very important point. Whether your unit is functioning at 60, 70, 80 or more occupancy while giving a measure of patient volumes tells you nothing about the coverage for such patients. In a well staffed unit with adequate nurse to patient ratios there might be minimal risk of error. If assignments though that are ideally 2:1 are stretched to 3 or 4: 1 that is likely where the errors start to come in.
Coming back to our situation that likely mirrors many other centres across the globe I believe all of this comes down to ensuring a safe environment to care for our patients. A safe environment means having enough staff to cover the number of patients and that includes medical, RRTs, dieticians and others. The message from all of this is that to do our best we need the right amount of staff to do it. We can handle the volume, just provide us with the resources to handle it. If it is money that we are hoping to save consider the amount of dollars that could be saved by avoiding prolonged stays from infection and all the associated morbidities that follow.
Then there is the increase in mortality to consider and I for one will not even begin to put a price on that.

by All Things Neonatal | May 19, 2016 | resuscitation, Uncategorized
As I was preparing to settle in tonight I received a question from a reader on my Linkedin page in regards to the use of sustained inflation (SI) in our units. We don’t use it and I think the reasons behind it might be of interest to others. The concept of SI is that by providing a high opening pressure of 20 – 30 cm H2O for anywhere from 5 to 15 seconds one may be able to open the “stiff” lung of a preterm infant with RDS and establish an adequate functional residual capacity. Once the lung is open, it may be possible in theory to keep it open with ongoing peep at a more traditional level of 5 – 8 cm of H20.
The concept was tested 25 years ago by Vyas et al in their article Physiologic responses to prolonged and slow-rise inflation in the resuscitation of the asphyxiated newborn infant. In this study, 9 newborn infants were given a relatively short 5 second sustained inflation and led to earlier and larger lung volumes with good establishment of FRC. Like many trials in Neonatology though sceptics abound and here we are 25 years later still discussing the merits of this approach.
As I have a warm place in my heart for the place that started my professional career whenever I come across a paper published by former colleagues I take a closer look. Such is the case with a systematic review on sustained inflation by Schmolzer et al. The inclusion criteria were studies of infants born at <33 weeks. Their article provides a wonderful assessment of the state of the literature on the topic and I would encourage you to have a look at it if you would like a good reference to keep around on the topic. What it comes down to though is that there are really only four randomized human studies using the technique and in truth they are fairly heterogeneous in their design. They vary in the length of time an SI was performed (5 – 20 seconds), the pressures used (20 – 30 cm H2O), single or multiple SIs and lastly amount of oxygen utilized being 21 – 100%. In fact three of the four studies used either 100% or in one case 50% FiO2 when providing such treatments.
What Did They Show?
This is where things get interesting. SI works in the short term by reducing the likelihood that an infant will need mechanical ventilation at 72 hours with a number needed to treat of only 10! In medicine we normally would embrace such results but sadly the results do not translate into long term benefits as the rate of BPD, mortality and the combined outcome do not remain significant. Interestingly, the incidence of a symptomatic PDA needing treatment with either a medical or surgical approach had a number needed to harm of 11; an equally impressive number but one that gives reason for concern. 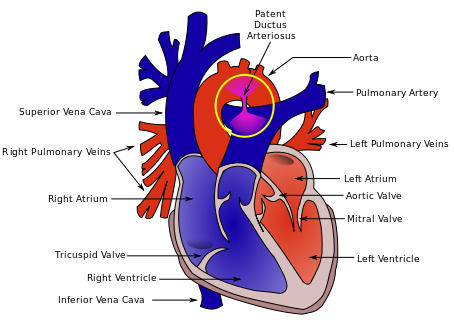 As the authors speculate, the increased rate of PDA may be in fact related to the good job that the SI does in this early phase. By establishing an open lung and at an earlier time point it may well be that there is an accentuation in the relaxation of the pulmonary vasculature and this leads to a left to right shunt that by being hemodynamically significant helps to stent the ductus open at a time when it might otherwise be tending to close. This outcome in and of itself raises concern in my mind and is the first reason to give me reason to pause before adopting this practice.
As the authors speculate, the increased rate of PDA may be in fact related to the good job that the SI does in this early phase. By establishing an open lung and at an earlier time point it may well be that there is an accentuation in the relaxation of the pulmonary vasculature and this leads to a left to right shunt that by being hemodynamically significant helps to stent the ductus open at a time when it might otherwise be tending to close. This outcome in and of itself raises concern in my mind and is the first reason to give me reason to pause before adopting this practice.
Any other concerns?
Although non-significant there was a trend towards increased rates of IVH in the groups randomized to SI. There is real biologic plausibility here. During an SI the increased positive pressure in the chest could well simulate a similar effect to a pneumothorax and impede the passive drainage of blood from the head into the thorax. In particular, longer durations and/or frequent SIs could increase such risk. Given the heterogeneous nature of these studies it is difficult to know if they all had been similar in providing multiple SIs could we have seen this cross over to significant?
I believe the biggest concern in all of this though is that I would have a very hard time applying the results of these studies to our patient population. The systematic review addresses the question about whether SI is better than IPPV as a lung recruitment strategy in the preterm infant with respiratory distress. I have to say though we have moved beyond IPPV as an initial strategy in favour of placement of CPAP on the infant directly after birth. The real question in my mind is whether providing brief periods of SI followed by CPAP of +6 to +8 is better than placement on CPAP alone as a first strategy to establish good lung volumes.
If I am to be swayed by the use of SI someone needs to do this study first. The possibility of increasing the number of hemodynamically significant PDAs and potentially worsening IVH without any clear reduction in BPD is definitely placing me firmly in the camp of favouring the CPAP approach. Having said all that, the work by the Edmonton group is important and gives everyone a glimpse into what the current landscape is for research in this field and opens the door for their group or another to answer my questions and any others that may emerge as this strategy will no doubt be discussed for years to come.

by All Things Neonatal | May 11, 2016 | drug withdrawal, NAS, Uncategorized
Original Post
I don’t know if you missed it but I did until tonight. We don’t have this in Canada but there have been some US states that have been doing so for the past while. You may find the following link very interesting that explains the positions of each state in regards to drug use in pregnancy. The intentions were good to protect the unborn child but the consequences to mother’s who tested positive were of great concern. While testing of mothers for drug use has been done off and on for years what made this different was that the confirmation of drug use was deemed to be a criminal offense with the results handed over to the police.
As this article from March 4th indicates the practice has been ongoing in Tennessee for at least a year and a pilot project was planned for Indiana this year. According to the article the situation in Tennessee came with some significant risk to the mother if found to have a positive screen.
“Lawmakers in Tennessee last year increased drug screenings of expectant mothers and passed a law allowing prosecutors to charge a woman with aggravated assault against her unborn baby if she was caught using illicit drugs. The penalty is up to 15 years in prison.”
The law may seem harsh and in my eyes is but it came in response to the tidal wave of drug addiction and neonatal withdrawal in the US as was identified in the article from the NEJM in 2015 entitled Increasing Incidence of the Neonatal Abstinence Syndrome in U.S. Neonatal ICUs. The impact on neonatal ICUs in the US can be seen in the following graphs which demonstrate not only the phenomenal rise in the incidence of the problem but in the second graph the gradually prolonging length of stay that these patients face. 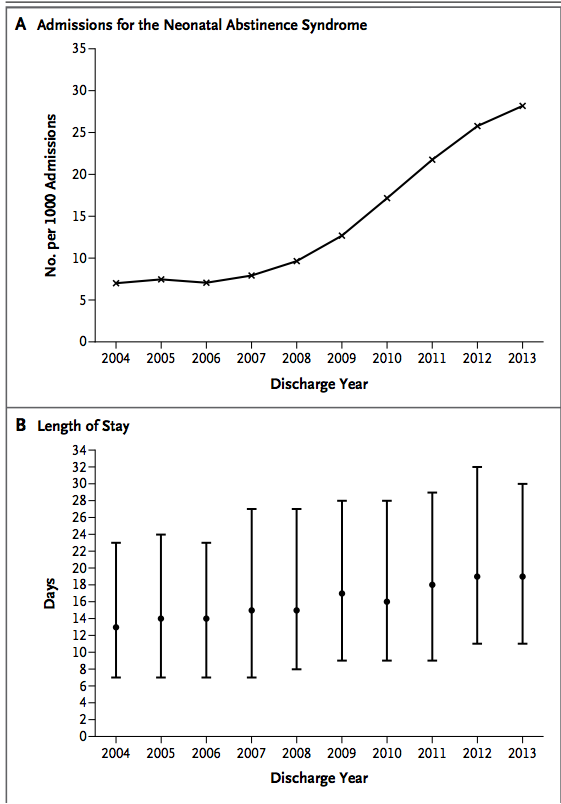 Aside from the societal issues these families face and the problems their infants experience, the swelling volume of patients NICUs have to contend with are quite simply overwhelming resources with time. Although I reside in Canada, it is the trend shown that likely motivated some states to adopt such a draconian approach to these mother-infant dyads.
Aside from the societal issues these families face and the problems their infants experience, the swelling volume of patients NICUs have to contend with are quite simply overwhelming resources with time. Although I reside in Canada, it is the trend shown that likely motivated some states to adopt such a draconian approach to these mother-infant dyads.
There are so many questions that would arise from such an approach.
- What if a mother refuses testing as is the option in Indiana. Would Child and Family services be called simply on the suspicion?
- What if a mother received prescription opioids for chronic back pain or used an old prescription in the days before she was tested after a fall to ease her pain?
- Then there is the Sharapova situation
 where a mother could conceivably take a medication that she is unaware is on a list of “banned substances”. What about Naturopathic or herbal supplements that might test positive?
where a mother could conceivably take a medication that she is unaware is on a list of “banned substances”. What about Naturopathic or herbal supplements that might test positive?
- Then what about false positive tests?
The ramifications of any of the above situations on the family unit could be devastating. Interestingly this year the courts in Indiana passed a law that prevents health care providers from releasing the results of such toxicology screens to police without a court order so indeed there would need to be suspicion. In the end though is it right?
Tennessee Sings a New Tune
As surprised as I was to hear about the situation in Tennessee just now I was equally surprised to come across a U.S. Supreme Court ruling handed down March 21st, 2001 that has ruled that subjecting mothers to such testing in hospitals is unconstitutional. This may disclose my ignorance of US law but I would have thought if the US Supreme Court says you cannot do something the states would follow along but at least in Tennessee that was not the case…until now.
March 23rd the law in Tennessee is changing as the state has chosen not to renew the legislation after a two year trial period saw about 100 women arrested. For more information on this decision see Assault Charges for Pregnant Drug Users Set to Stop in Tennessee.
Where do we possibly go from here?
I found this whole storyline shocking but I am taking some solace in knowing that this was a very limited experiment in one state. Neonatal abstinence is a problem and a big one at that. Criminalizing mothers though is not an effective solution and to me the solution to this problem will need to involve a preventative approach rather than one of punishment. A first step in the right direction will be to stem the tide of liberal use of prescription opioids in pregnancy as was suggested in the BMJ news release in January of this year. In the end if we as medical practitioners are freely prescribing such medications to the mothers we care for perhaps we should look in the mirror when pointing fingers to determine fault. So many of the mothers and the infants we care for may well be victims of a medical establishment that has not done enough to prevent the problem.
Update
While screening women presenting to the hospital in labour or their newborns for that matter may seem like a wise choice, the request to procure a sample remains just that. It is a request and in collecting consent is needed. This was the advice at least I was given by the Canadian Medical Protective Association. It does create an interesting situation though in the mother who refuses to have her or her baby submit a urine specimen. Should we assume that a woman who refuses testing is in fact using an illicit substance or is she merely choosing to not have a wasted test when she knows that she is not using anything? How do we as practitioners view this decision and do we jump to a verdict of guilt immediately? I suspect the answer is that most of us would assume so especially if we are using a targeted screening approach in which we are only approaching those mothers who we suspect are using.
The secondary question becomes the “so what”? What I mean by this is how will our management change if we know or don’t know? If we suspect use and the baby is demonstrating signs of withdrawal abstinence scoring will start. If the source of the symptoms are unknown would we not just treat with phenobarbital to cover the possibility that there is more than one drug at play here? I used to be on the side of the argument that felt we had to know and therefore pushed for such screening but in the end will it really change our management? Not really.
This past month the American College of Obstetricians and Gynecologists (ACOG) issued a committee opinion on opioid use in pregnancy. The important points to share with you are the following and I would agree with each.
- Screening for substance use should be part of comprehensive obstetric care and should be done at the first prenatal visit in partnership with the pregnant woman. Screening based only on factors, such as poor adherence to prenatal care or prior adverse pregnancy outcome, can lead to missed cases, and may add to stereotyping and stigma. Therefore, it is essential that screening be universal
- Urine drug testing has also been used to detect or confirm suspected substance use, but should be performed only with the patient’s consent and in compliance with state laws.
- Breastfeeding should be encouraged in women who are stable on their opioid agonists, who are not using illicit drugs, and who have no other contraindications, such as human immunodeficiency virus (HIV) infection. Women should be counseled about the need to suspend breastfeeding in the event of a relapse.
The issue of consent seems to be firmly in place based on this position and as I mention above I think that is a good thing. The question of breastfeeding comes up frequently and it is good to see ACOG take a clear view on this as I have often thought that the benefits of the same plus the administration of small quantities of the drug in the milk may have a double benefit in reducing symptoms.
.

by All Things Neonatal | May 4, 2016 | congenital heart defects, Uncategorized
As evidence mounts for the use of pulse-ox screening to detect congenital heart defects a few key points have arisen. The evidence comes from many publications but one of the best which summarizes the body of evidence is the systematic review by Thangaratinam S which included over 200000 asymptomatic newborns. The key here is to note that as this is a screening test if there are symptoms of congenital heart disease one should be referring to a specialist to rule out a significant CHD rather than spending time with such screening tests. The four points to highlight though are:
- Comparing preductal to postductal saturations enhances sensitivity
- Performing such testing after 24 hours decreases false positive results from conditions leading to desaturation that are not CHD such as TTN.
- The false positive rate is 0.14% if the first two criteria are applied using the cutoffs of < 95% in any limb or > 3% difference between pre and post ductal locations.
- Pulse-ox screening does not detect ALL CHD but rather the ones that are deemed critical or immediately life threatening if not identified in the newborn period.
| Examples of CCHD Lesions Detectable with Pulse Oximetry Screening |
| Most consistently cyanotic |
May be cyanotic |
| Hypoplastic left heart syndrome (HLHS)
Pulmonary atresia with intact septum (PA IVS)
Total anomalous pulmonary venous return (TAPVR)
Tetralogy of Fallot (TOF)
Transposition of the great arteries (TGA)
Tricuspid atresia
Truncus arteriosus |
Coarctation of the aorta (COA)
Double outlet right ventricle (DORV)
Ebstein anomaly
Interrupted aortic arch (IAA)
Single ventricles
|
Is there a danger in screening too early?
As you screen closer to birth the risk of detecting conditions leading to desaturation which are not CHD rises. Common conditions such as TTN or mild pulmonary hypertension may mimic CHD and lead to a false positive finding. Thinking of the hospital environment, how many patients are sent to triage beds on a daily basis with tachypnea and mild desaturation?
This month the first real assessment of screening in the home environment was completed by Cawsey MJ entitled Feasibility of pulse oximetry screening for critical congenital heart defects in homebirths. This study describes in a retrospective fashion the results of applying a pulse-ox screening protocol in the UK to 90 babies screened at 2 hours of age. This study is important as the typical early discharge of patients from birth centres or could potentially benefit as well by having the results of such work available. Out of the 90 patients screened 4 had abnormal results and after rescreening two were normal but 2 were persistently abnormal and required admission for further workup. Neither of the two had CHD but were diagnosed with congenital pneumonia.
This yields a false positive rate of 2% or about 16 times as high as screening after 24 hours.
How do we apply the results?
As the saying goes “something is better than nothing”. In the home or birthing centre environment, waiting until after 24 hours to perform the screen may not be possible either due to the midwife leaving after the delivery or in the case of a birth centre the couple leaving before 6 hours as is the case in our local centre. As I see it all is not lost in doing screening in such circumstances early as one may detect TTN, pneumonia or another vascular condition such as PPHN before it becomes symptomatic. Intervening earlier in the course of the illness may actually result in better outcomes for the infant. We have to be careful though when looking at the ability of this screen to detect CHD. The truth is there are not enough patients screened in this study to really draw any conclusions. With an incidence of about 1:100 births a sample of 90 patients would be lucky to find one patient so the absence of any detected patients is not surprising.
The study though does draw attention to a couple important points. First as mentioned above, the midwife has the opportunity by screening early to detect ANY cause of desaturation and then plan for further management. Secondly, it does raise the question with a 2% false positive rate whether screening programs regardless of home or birth centre should include follow-up by a midwife after 24 hours to do testing. My vote would be a resounding yes. If applied to a population there would certainly be kids detected with CHD over time and reducing the false positive rate is important in terms of the downstream consequences of overwhelming our Cardiology colleagues who would ultimately need to see such patients to rule in or out significant CHD.
I am not a midwife, nor do I attend home or birthing centre deliveries but I would ask that the consideration of such screening programs consider the timing of testing as sending 2 per 100 deliveries vs 1 in 1000 deliveries for further assessment to rule out CHD is something that our overwhelmed health care systems need to consider strongly.

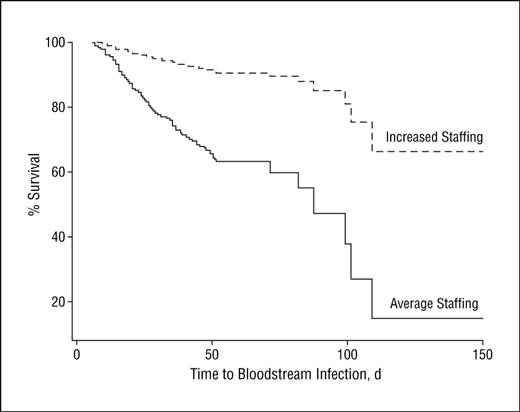 Looking also at the impact of greater nursing hours on time to infection demonstrated the following curve. From the graph one can see that two patients both of which develop an infection at 100 days of life have markedly different chances of survival based on the staffing level. The Neonatologist, RRT, dietician could all be the same but if the nursing hours are lacking the patient is more likely to die. A very significant concern indeed!
Looking also at the impact of greater nursing hours on time to infection demonstrated the following curve. From the graph one can see that two patients both of which develop an infection at 100 days of life have markedly different chances of survival based on the staffing level. The Neonatologist, RRT, dietician could all be the same but if the nursing hours are lacking the patient is more likely to die. A very significant concern indeed!

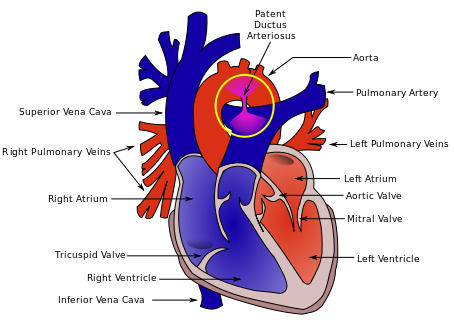 As the authors speculate, the increased rate of PDA may be in fact related to the good job that the SI does in this early phase. By establishing an open lung and at an earlier time point it may well be that there is an accentuation in the relaxation of the pulmonary vasculature and this leads to a left to right shunt that by being hemodynamically significant helps to stent the ductus open at a time when it might otherwise be tending to close. This outcome in and of itself raises concern in my mind and is the first reason to give me reason to pause before adopting this practice.
As the authors speculate, the increased rate of PDA may be in fact related to the good job that the SI does in this early phase. By establishing an open lung and at an earlier time point it may well be that there is an accentuation in the relaxation of the pulmonary vasculature and this leads to a left to right shunt that by being hemodynamically significant helps to stent the ductus open at a time when it might otherwise be tending to close. This outcome in and of itself raises concern in my mind and is the first reason to give me reason to pause before adopting this practice.
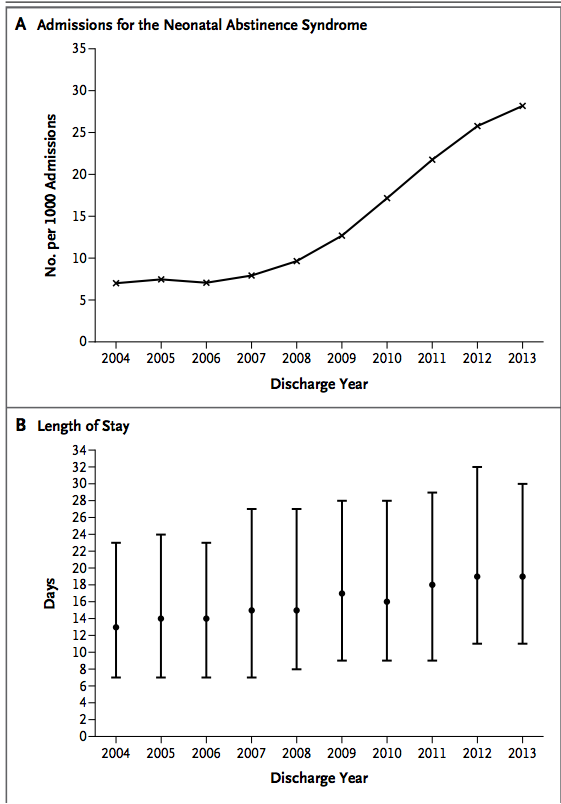 Aside from the societal issues these families face and the problems their infants experience, the swelling volume of patients NICUs have to contend with are quite simply overwhelming resources with time. Although I reside in Canada, it is the trend shown that likely motivated some states to adopt such a draconian approach to these mother-infant dyads.
Aside from the societal issues these families face and the problems their infants experience, the swelling volume of patients NICUs have to contend with are quite simply overwhelming resources with time. Although I reside in Canada, it is the trend shown that likely motivated some states to adopt such a draconian approach to these mother-infant dyads. where a mother could conceivably take a medication that she is unaware is on a list of “banned substances”. What about Naturopathic or herbal supplements that might test positive?
where a mother could conceivably take a medication that she is unaware is on a list of “banned substances”. What about Naturopathic or herbal supplements that might test positive?