I feel like this has been a story in the making for some time. Next to caffeine, the story of prophylactic hydrocortisone must be one of my more popular topics and has been covered more than once before as in A Shocking Change in Position. Postnatal steroids for ALL microprems or Early Hydrocortisone: Short term gain without long term pain. and the last post Hydrocortisone after birth may benefit the smallest preemies the most! After reporting on this topic about once a year, a recent paper may wrap it all up in a bow for the holidays and present to us the conclusion after all this work on the topic. I was extremely interested in this topic not just because I believe this therapy may have a future in the standard approach to neonatal care for VLBWs but because I have served on the CPS Fetus and Newborn committee with two of the authors of the paper. Dr. Lacaze and Dr. Watterberg have an exceptional understanding of this topic and so when they band together with other experts in the field I take notice.
An Individual Patient Data Meta-Analysis
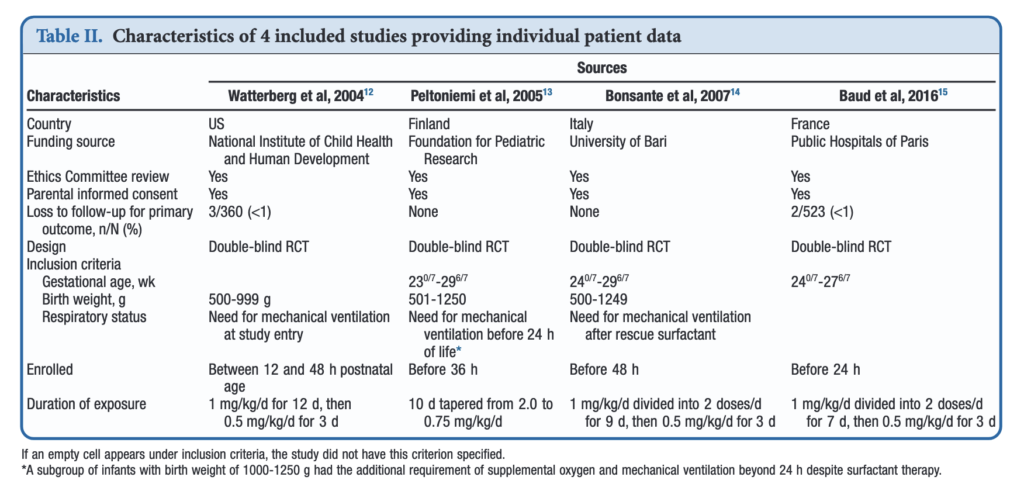
If you have read my previous posts then you know the story of why hydrocortisone given over the first 10-12 days of life might help those born before 30 weeks or < 1250g. In essence the concept is that it has been shown previously that many infants with relative adrenal insufficiency may go on to develop BPD. If you treat all such infants at risk you could theoretically reduce BPD. Typically after a few studies examining a similar topic come out, one can combine them in a meta-analysis using aggregate data (averages of effect sizes for the individual studies) and see what the larger sample shows. Another way to do it though is to go back to the original data and examine the infants at a more granular level allowing a greater identification and control of variables that might influence outcomes. This is what the authors led my Michele Shaffer did here in the paper Effect of Prophylaxis for Early Adrenal Insufficiency Using Low-Dose Hydrocortisone in Very Preterm Infants: An Individual Patient Data Meta-Analysis. There were a total of 5 studies on this topic but one study of 40 patients no longer had individual data so was excluded from analysis leaving 4 to look at. The details of the four studies are shown below. You can see that the inclusion criteria differed slightly but in general these were all infants up to 27 – 29 completed weeks and 500 – 1250g maximum who were treated with regimens as shown in the table.
What were the results?
Treatment with early low-dose hydrocortisone was associated with greater odds of survival without BPD at 36 weeks PMA after adjustment for sex, gestational age, and antenatal steroid use (aOR, 1.45; 95% CI, 1.11-1.90; I 2 = 0%). Also found were lower individual odds of BPD (aOR, 0.73; 95% CI, 0.54-0.98; I 2 = 0%), but not with a significant decrease in death before 36 weeks PMA (aOR, 0.76; 95% CI, 0.54-1.07; I 2 = 0%). Importantly although death by 36 weeks was not different, a decrease in death before discharge (aOR, 0.70; 95% CI, 0.51-0.97; I 2 = 0%) was found. Also noted and important was a reduction in medical treatment for PDA OR 0.72 (0.56-0.93)
All of these outcomes sound important but in a subgroup analysis other interesting findings emerged.
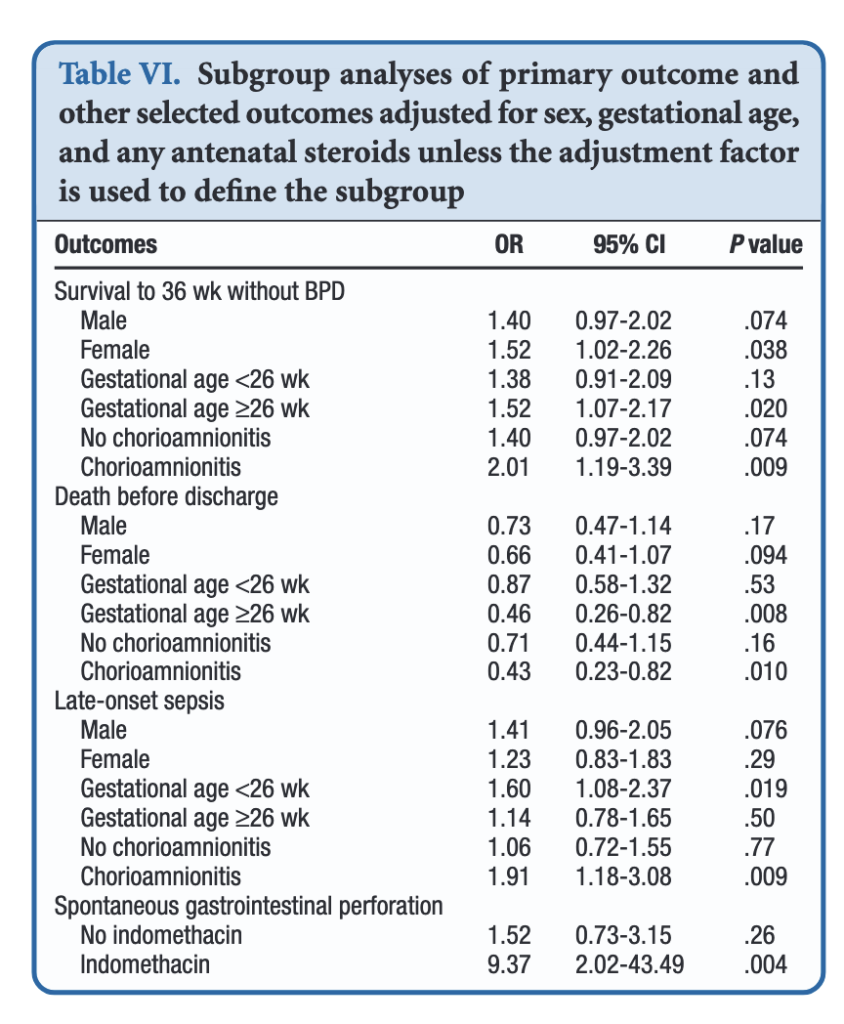
When dividing the patients into those less then 26 weeks and those at or greater than that gestational age, the benefits appear to be limited to those in the latter group. Levels of significance are high once you reach that GA suggesting that issues affecting those at younger gestational ages are less amenable to treatment. On the other hand one could say that the benefits seen at 26 – 29 weeks GA are relatively strong using a glass is half full approach. An important outcome worth noting is that while spontaneous intestinal perforation is noted to be a risk with prophylactic hydrocortisone, when you remove indomethacin from the equation the risk disappears. For those units using prophylactic hydrocortisone one would likely need to choose between the two but if you are like our unit where we don’t have that option this may be one strategy to consider.
In terms of risk to giving such therapy the big one noted in the paper was an increase in risk for late onset sepsis. Interestingly, this was limited though to the group under 26 weeks GA. In essence then the messaging would appear to be that under 26 weeks there may be less benefit to such treatment and therefore the increased risk of late onset sepsis without such benefits on BPD would suggest not using it in this GA group.
Where do we land then?
It would be easy to cast this aside I suppose as the group you are most worried about (22-25 weeks) doesn’t seem to really benefit but has a risk of late onset sepsis. That leaves us though with the group from 26-29 weeks. They do seem to benefit and may do so to a significant degree. They do develop BPD and to be honest we don’t have much outside of trying our best to use gentle ventilation to ameliorate their course in hospital. It is worth noting that the one group that does seem to show the greatest benefit are those exposed to chorioamnionitis. It is this group in particular that may be the best target for this intervention and I gather this has been discussed at a recent EPIQ meeting.
If one says no to trying this approach then the question that needs to be asked is whether doing nothing for this group is better than supporting them with hydrocortisone? If your centre’s rates of BPD are top notch then maybe you don’t want to add something in. If not though maybe it is time to rock the boat and try something different.

