Breast milk is certainly a hot topic these days. Allergies in childhood are almost equally hot in the media as food allergies seem to be on the rise (not my specialty by a long shot) as well as rates of other atopic illness. Given what is known about the modifiable risks in terms of a number of conditions such as NEC and late onset sepsis in preterm infants it wouldn’t be a stretch to wonder what impact avoidance of cow’s milk exposure could have in the term newborn.
A Landmark Japanese Study
Urashima et al just published in JAMA Pediatrics the following paper Primary Prevention of Cow’s Milk Sensitization and Food Allergy by Avoiding Supplementation With Cow’s Milk Formula at Birth: A Randomized Clinical Trial . This paper looked at 312 infants (≥ 36 weeks at birth) who were randomized to either receive breastfeeding plus an elemental formula if needed vs breastfeeding plus intact protein cow’s milk formula with a volume of at least 5 mL/kg per day. In order to have a group of infants truly at risk of atopic disease, all infants had to have at least one immediate relative with atopic disease. In each arm of the study, infants were followed with blood IgE levels at 5 and 24 months of age to detect a level of CM-IgE ≥ allergen units/mL. This was the primary outcome on which the power calculation was based for the study. Using an estimated incidence of 10% in the breastmilk group vs 25% in the exposed group the authors needed 300 patients to detect a difference. Secondary outcomes included detection of other allergens aside from allergy to cow’s milk.
The Findings
Given that I called this a landmark study it might not be surprising to know that they found a difference favoring protection with human milk.
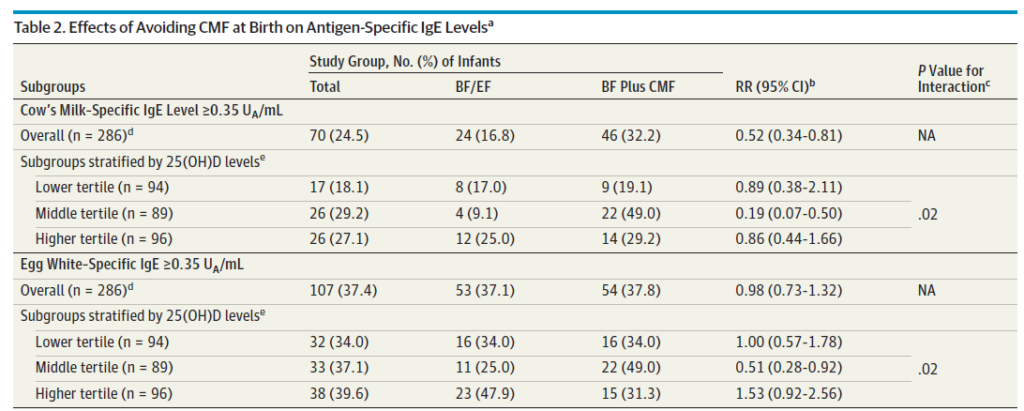
Also curious is the relationship to vitamin D levels. Previous research has documented an inverse relationship between vitamin D levels in children and risk of atopy. Why only the middle tertile in this study but not the higher tertile had less IgE response is unknown.
Perhaps even more surprising (at least to me) was that the risk of allergy at age 2 for other allergens was also lower.
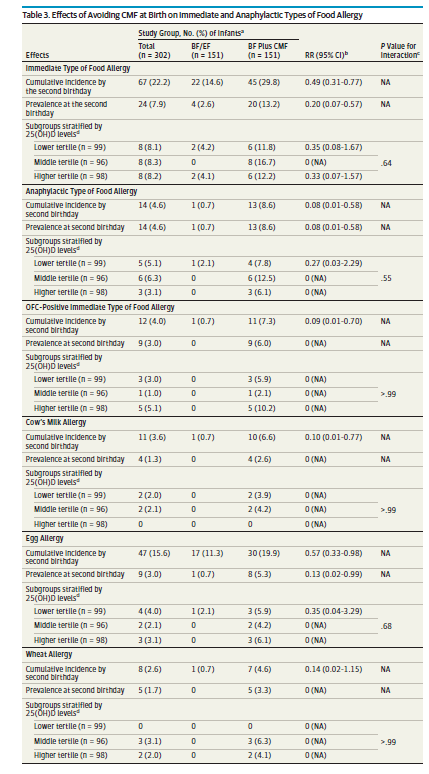
Included in this lower risk was food allergy in general, risk of anaphylaxis and cow’s milk allergy that I presume manifested as rectal bleeding.
What Impact Could This Have
It is important to point out here that all these infants were ≥ 36 weeks so although I would love to infer that this strategy would have a huge impact on our preterm population I can’t say that yet (until a study is done). We certainly do see a fair bit of cow’s milk protein intolerance though that often leads to infants being placed NPO and on occasion worked up for NEC with a week or so of antibiotics. If this study is to be trusted, the rate of cow’s milk allergy was reduced from 6.6% to 0.7% in at risk infants (based on an immediate relative with atopy) and I would expect the risk in those without relatives to be less.
What might the impact be if we were to supplement with donor breast milk all term newborns who didn’t have enough maternal milk and take the elemental formula out of the equation entirely? If a 4 kg infant exclusively breastfed on day 1 and was give a couple ounces of supplement followed by full supplementation to 80 mL/kg/d on day 2 and then 100 mL/kg/d on day 3 that would total 26 ounces of donor milk in a worst case scenario assuming no maternal milk production during that time. At $4 per ounce we are looking at a cost to the system of about $100 a baby. Multiple that by the number of term infants in your centre to get an overall cost. In my own centre with about 12000 term deliveries a year that would come to 1.2 million dollars a year (again assuming no maternal milk at all). Is it worth the expense? I am not a health economist but I suspect if you were to add up the costs of workups/office visits etc for rectal bleeding, ED visits for asthma and anaphylaxis and the cost to families for food alleriges (let alone all the epi pens that need to be bought) it is worth it.
At the very least it does raise the question on post partum wards everywhere as to whether provision of cow’s milk formula should be one that someone has to consent to. With the publication of this study it certainly seems that it should be!

