by All Things Neonatal | Aug 5, 2016 | Uncategorized
There may be nothing that is harder in medicine. We are trained to respond to changes in patients condition with a response that more often than not suggests a new treatment or change in management. Sometimes the best thing for the patient is in fact to do nothing or at least resist a dramatic response to the issue in front of you. This may be the most common issue facing the new trainee who is undoubtedly biased towards doing something. Take for instance the situation in which the trainee who is new to the service finding out that their 26 week infant has a PDA. Their mind races as they digest this information from morning signover. There is less than 2 hours until they come face to face with their attending who no doubt will ask them the dreaded question. “What are you going to do about it?”. When having to choose a path, if they state “I want to sit tight and watch” they fear the thought of the attending thinking they don’t know what to do. Conversely they could stick their neck out and choose to treat with a variety of approaches but then might they be seen as too aggressive?! The likely path is suggesting treatment but in fact the more I think about it the option of benign neglect may be the best approach or at least one in which if you treat and it doesn’t work the first time you just shrug your shoulders and say “I’ll deal with it till it closes on it’s own”.
This post really is a follow-up to a previous one entitled The Pesky PDA. A Puzzle After All These Years. What triggered this writing was another before and after comparison of two periods in which the management of PDAs for a unit took a 180 degree turn.
Know When to Hold Em And No When to Fold Em
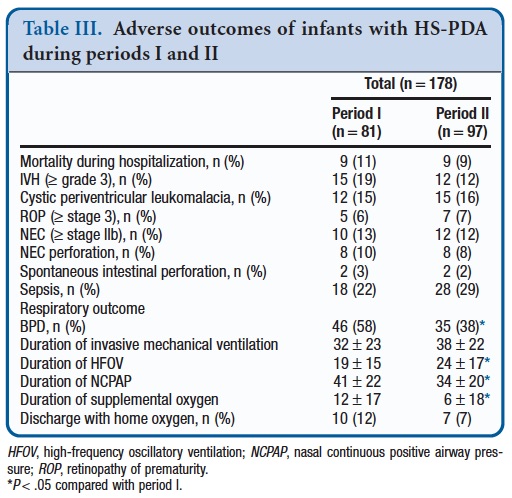
This is the essence of the issue for one unit. Sung SI et al published a paper this month entitled Mandatory Closure Versus Nonintervention for Patent Ductus Arteriosus in Very Preterm Infants. They describe a before and after comparison of 81 infants from 2009-11 and 97 infants from 2012-14. All babies were born between 23-26 weeks gestational age. In the first time period their unit had a mandatory PDA closure policy. That is they gave one course of indomethacin and if possible a second course followed by surgical ligation. A significant PDA was defined as one that had a left to right shunt and was at least 2 mm in diameter and the patient had to be ventilated. Any patient who had been extubated regardless of need for CPAP did not have to have their PDA closed. In the second time period the group attempted to avoid indomethacin and ligation at all costs and in fact in this cohort none received either.
So What Happened?
In the first time period 52 (64%) received indomethacin but only 29% responded and a full 37/52 (71%) went on to receive surgical ligation. Of the 29 that did not receive indomethacin due to contraindications they underwent primary ligation for a total of 82% receiving surgical ligation. The average day of closure for period 1 was 12.9 days.
In period 2 a number of interesting findings occurred. The average day of closure was at 44.2 days. Five infants were discharged with a PDA with 3 experiencing spontaneous closure after discharge and the remaining infants undergoing transcatheter occlusion. In period 2 there were more diuretics and fluid restriction employed. Comparing the two periods for a number of other outcomes reveals some other intriguing findings.
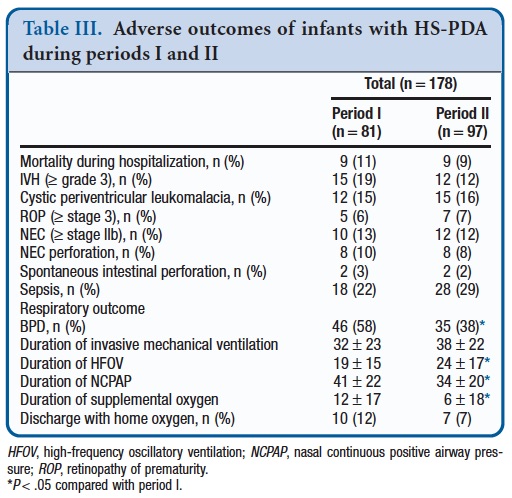
Even with such differing approaches there is no difference in mortality, severe IVH, ROP, PVL, NEC or sepsis. What is different though is the diagnosis of BPD yet there is no difference in total ventilation. In period 2 there is a shift towards more of this ventilation being HFOV less CPAP use at the same time.
What Might It All Mean?
It is retrospective and therefore we cannot be certain that there are not other variables that are not affecting the results that would have had a better chance of being evened out in an RCT. Having said that it is intriguing that having a PDA has been associated with BPD in the past but in this study having a PDA for a longer time is associated with a reduction in BPD. We know that longer periods of invasive mechanical ventilation increase the risk of developing BPD so it is intriguing that that there is no difference in mechanical ventilation yet there is more BPD when you are aggressive with the PDA. You might postulate that the need for surgery leads to greater need for ventilatory support and therefore damages the lungs but the needs for HFOV was higher in the second phase which at least hints that in terms of aggressiveness, Period 2 infants had a tougher go.
The culprit may be the heart. In period 1 there was a significantly increased rate of myocardial dysfunction and need for inotropes following ligation. It could well be that left ventricular dysfunction led to pulmonary edema such that in the 24-28 hours after the surgery ventilator requirements were increased and damaged the lung. The lack of a difference in overall ventilation days supports this possibility. Looking at the other common risk factors for BPD such as chorioamnionitis and lack of antenatal steroids these are no different between groups. Although not statistically significant there are more male infants in period 2 which would usually tip the scales towards worse outcome as well. It does need to be stressed as well that the rate of surgical ligation is higher than any study I have come across so the contribution of the surgery itself to the disparate outcome needs to be seriously considered.
What would I do?
Despite this study and some others that have preceded it I am not at the point of saying we shouldn’t treat at all. Our own approach is to give prophylactic indomethacin to such babies and then for the most part if a PDA remains treat one more time but at all costs try and avoid ligation. An RCT sounds like it is in the works though comparing the two approaches so that will certainly be interesting to see. It is tough to say what the future holds but to any young trainees who are reading this, the next time you are asked what to do about a PDA you are well within your rights to suggest “Maybe we should do nothing”!

by All Things Neonatal | Jul 28, 2016 | surgery, transfusion, Uncategorized
A 28 week preterm infant now two weeks of age develops bilious emesis and abdominal distension. An x-ray reveals an intestinal perforation and surgery is consulted. Arrangements are made to go to the operating room for a laparotomy and due to apnea and hypotension the baby is both intubated and placed on dopamine. The resident on service ensures that blood is available in the operating room and an hour after presentation the baby is found to have a HgB of 102 g/L with a HcT of 35%.
I don’t know about you but if I am then asked whether we should give blood now or in the OR I might say at that level with the degree of illness to give blood or I might say wait till the baby gets to the OR if perhaps they were fairly stable on the support.  You the reader might be more convinced of your actions but if I manipulate the numbers a little bit to say 105 g/l and HcT of 37% might you feel different? What about 110 g/L and 39%? You get the picture. Where is that magic cutoff where we say prior to an OR that a baby needs blood or can wait? In our heads of course we conjure up the equation for delivery of O2 to tissues Cardiac output X (1.39 X HgB X Sat +0.003*pO2) and realize that the delivery of oxygen is critically dependent on HgB level but how much is enough? The truth is I don’t think we really know but we do a good job of coming up with some markers such as lactate or more recently near infrared spectroscopy to give us an idea of how much O2 the tissues are seeing.
You the reader might be more convinced of your actions but if I manipulate the numbers a little bit to say 105 g/l and HcT of 37% might you feel different? What about 110 g/L and 39%? You get the picture. Where is that magic cutoff where we say prior to an OR that a baby needs blood or can wait? In our heads of course we conjure up the equation for delivery of O2 to tissues Cardiac output X (1.39 X HgB X Sat +0.003*pO2) and realize that the delivery of oxygen is critically dependent on HgB level but how much is enough? The truth is I don’t think we really know but we do a good job of coming up with some markers such as lactate or more recently near infrared spectroscopy to give us an idea of how much O2 the tissues are seeing.
How much HgB does a baby need before surgery?
Although this may seem like something that is well known, the truth is we don’t really know. We may have an inkling though based on a recent paper entitled Association of Preoperative Anemia With Postoperative Mortality in Neonates by S. Goobie et al. They performed a retrospective review of a US surgical quality database to examine mortality after operations and identified 2764 neonates out of 114395 children who underwent surgery. Similar to previous studies the neonatal postoperative mortality rate was higher at 3.4% than the rest of childhood at 0.6%. When examining the effect of low hematocrit prior to surgery they further identified a cutoff of 40% below which the risk of mortality increased. Of the neonatal group that survived 31% had a preop hematocrit of 40% or more while of those who died 72% had a hematocrit < 40%.
Hematocrit was not the only factor predicting mortality though as ASA class 3 – 5 (an anesthesiology risk score where these scores indicate severe systemic disease or emergencies), weight < 2 kg, preoperative ventilation and inotropic support. Put simply, sicker small patients have worse outcomes which I suppose should not surprise anyone.
So how do we interpret this data?
One important point that this article does not control for is the specific type of condition that the patient had. Clearly all conditions of the newborn are not the same as for example an umbilical flap closure of gastroschisis compared to fulminant necrotizing enterocolitis. The authors do try and control somewhat for this by demonstrating that the ASA categories demonstrate if you have severe systemic disease you are worse off but where does this leave the hematocrit? The other possible explanation is that the anemia is simply a reflection of the critical nature of the patient. Sicker patients are more likely to be anemic and also patients who present later are as well. A baby needing a colostomy for a bowel obstruction diagnosed after birth is likely to have low risk of mortality and also have a normal HgB. Contrast this with the baby who develops NEC at 3 weeks of age who is likely anemic or close to being so when they present and in the presence of shock and DIC becomes even more so. Is the low HcT just a proxy for severity of disease?
I suspect for the otherwise well infant who is electively intubated for surgery, having a hematocrit alone below 40% is not dangerous. What do we do though with the baby who is on inotropes for example. To truly answer this question we need a randomized controlled trial comparing transfusing patients with a hematocrit below 40% vs choosing a higher threshold of say 50% to say whether it makes a difference. That doesn’t help us though in the here and now. This gold standard for studies won’t tell me what to do for a few years but right now I have to decide what to do for a patient in front of me.
Not everyone may agree with me on this but I think in such circumstances I would transfuse based on this publications results. To the naysayers out there I would suggest that whether I choose to give the blood or not before the operation, they will be getting it after they enter the OR. Why not give them a boost before they undergo the knife? It is not a question of whether they will be transfused or not it is a difference in time.
If I have the chance I will “top them up” but what will you do?

by All Things Neonatal | Jul 21, 2016 | Intravenous access, Uncategorized
As with many things in Neonatology, changes in practice come and go. Such is the case with how best to manage an IV. During my career I have seen advocates for both continuous infusions and intermittent flushing. Sometimes with heparin and at other times none. The issue at hand is how best to preserve the precious IV. Based on opinion only I would have said that having a continuous flow through a plastic catheter should help avoid clot formation and prolong the life of an IV but what is the actual evidence to support one method or the other.
Why might flushing be better?
Clotting may not be the biggest issue to contend with. When I think about the IVs that are “lost” I am more commonly approached by nurses with concerns that the site is looking “red” and ultimately becomes indurated as the catheter extravasates. Far less common, is a concern that the catheter has simply obstructed or is reading high resistance these days. While we flush IVs with isotonic saline, infusions of dextrose are both hypotonic and acidic which may lead to endothelial damage. In theory then phlebitis should be lessened with intermittent flushes but could blockage due to clots still be an issue if there is no flow at the tip and lumen of the catheter?
What does the evidence show?
In 2012 Perez A et al looked at this in their paper Intermittent flushing improves cannula patency compared to continuous infusion for peripherally inserted venous catheters in newborns: results from a prospective observational study. As with the few recent papers out there on the subject, the study was small and performed over one year as an observational cohort. Out of 53 patients with 86 cannula insertions 25 had continuous dextrose infusions vs 28 who received at least one flush with NS per day. The findings in this study were that the mean cannula patency was 62.1 hr in the continuous group vs 92.8 hrs in the flushing group. Given the size of the study it might not be too surprising that practice did not change but that is where a more recent study may add some strength.
A more recent paper by Stok and Wieringa adds to this discussion by looking exclusively at the use for durations of antibiotics (Continuous infusion versus intermittent flushing: maintaining peripheral intravenous access in newborn infants). As with the previous study this was an observational cohort in which a shift in practice occurred from use of continuous 5% dextrose infusions to flushing six times per day with NS through a 24 gauge IV. The primary outcome was duration of catheter patency but several other important outcomes were followed as well in particular the time required by nursing to deal with IV issues.
A total of 115 newborns were recruited with 98 completing the analysis after excluding some patients. Of these newborns 71 fell into the continuous infusion vs 62 cannulas in the flushing cohort. Interestingly the main outcome was found to be no different between groups (55.42 hrs flushing vs 57.48 hrs continuous) regardless of placement site. Also interesting is that the median number of cannula placements were no different as well.
With respect to complications the results indicate that this is more of an issue with continuous infusions and is shown in the table below. The differences in complication rates were significant between the two groups. Consistent with endothelial damage being more common from dextrose infusions, the incidence of phlebitis and infiltration were both higher in the continuous group. Arguably this was not a blinded study so the diagnosis of phlebitis could be subject to bias but infiltration should have been more objective.
The amount of time nursing spent addressing IV related activities was significantly shorter with 8.8 minutes per shift vs 5.5 minutes in the continuous vs flushing groups respectively. Statistically significant but perhaps not that clinically relevant. Then again the extra three minutes of aggravation might be quite significant!
Finally, it may be surprising that the length of IV patency was no different between the groups but the majority of the IVs were utilized for less than 48 hours so one can only speculate what would have happened if a different target population was looked at such as babies being treated with peripheral IVs for 7 days of antibiotics as an example. Given the differing rates of complications I would think that with longer use a difference in mean durations of patency would in fact present itself.
What does the future hold?
This is hard to say. Opinions run strong on this topic with most members of the medical team favouring continuous infusions as they “don’t want to lose the IV”. I suspect the way to truly look at this will not be through a randomized trial but rather a quality project in which a formal PDSA cycle is utilized to first collect our own numbers and then implement a formal change to using flushing only for those who only have an IV for antibiotics. Certainly something to discuss with our group and perhaps your own. If you have already done such a project and wish to share the results I would love to hear from you though!

by All Things Neonatal | Jul 9, 2016 | preemie, Prematurity, Uncategorized
Preterm infants born between 22 to 25 weeks gestational age has been a topic covered in this blog before.
I think it is safe to say that this topic stirs up emotions on both sides of the argument of how aggressive to be when it comes to resuscitating some of these infants, particularly those at 22 and 23 weeks. Where I work we have drawn a line at 23 weeks for active resuscitation but there are those that would point out the challenge of creating such a hard-line when the accuracy of dating a pregnancy can be off by anywhere from 5 – 14 days. Having said that, this is what we have decided after much deliberation and before entertaining anything further it is critical to determine how well these infants are doing not just in terms of survival but also in the long run. In the next 6 months our first cohort should be coming up for their 18 month follow ups so this will be an informative time for sure.
Do Days Matter?
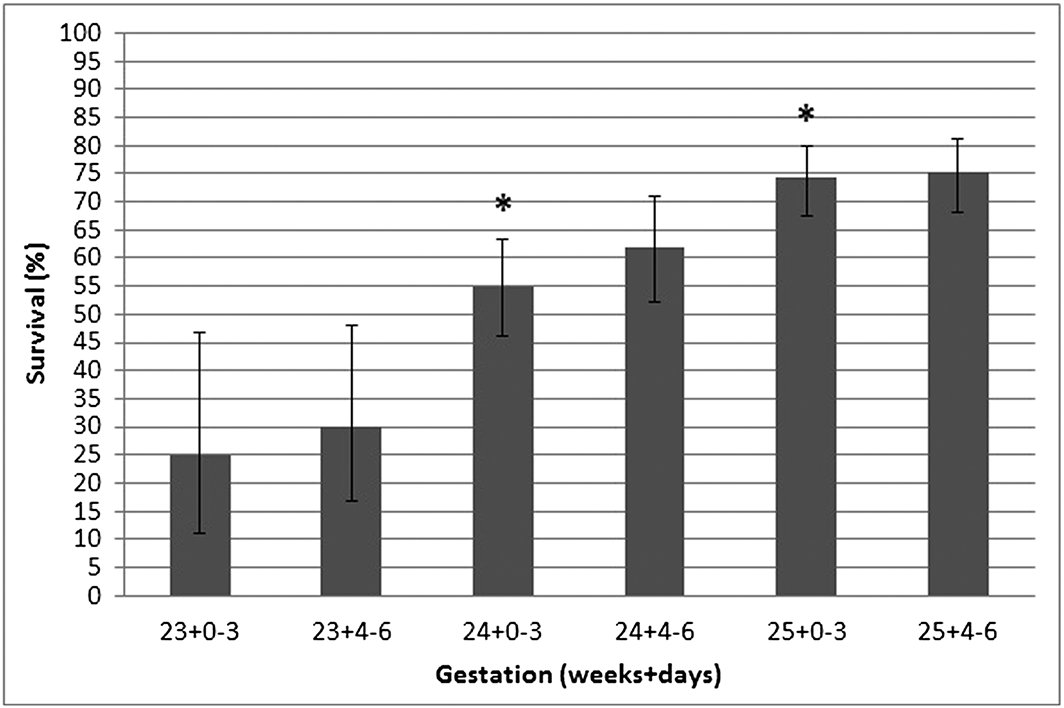
This is the subject of a short report out of Australia by Schindler T et al. In this communication they looked at the survival alone for preterm infants in a larger study but broke them down into 3 and four-day periods from 23 to 25 weeks as shown below.
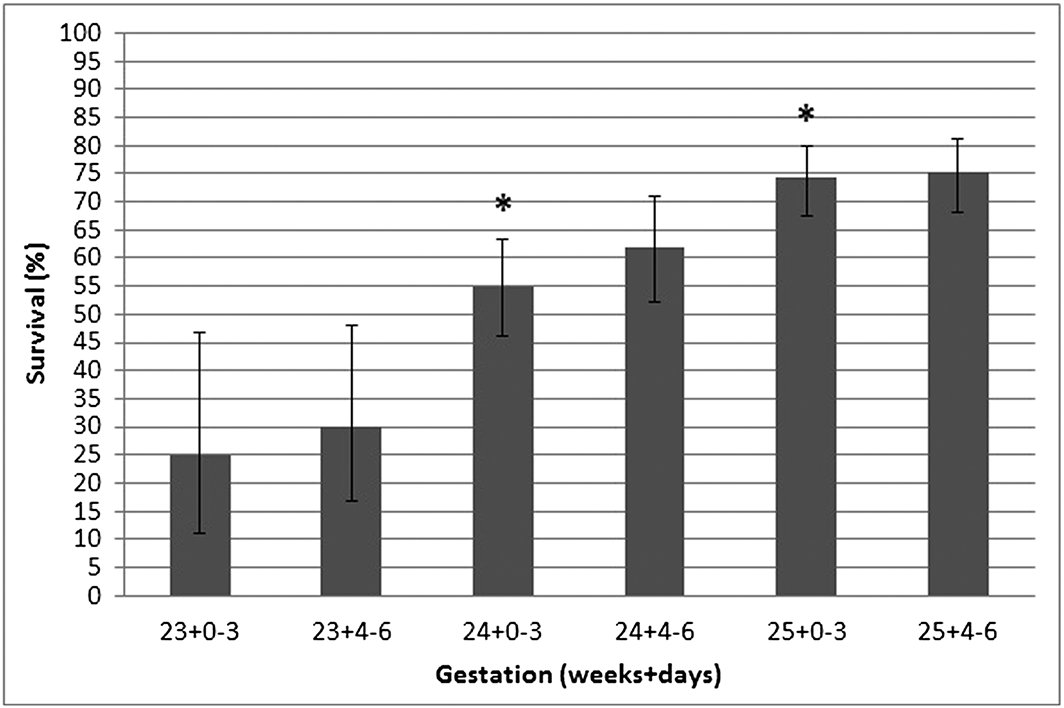
The asterisk over the two bars means that the improvement in survival was statistically significant between being born in the last half of the preceding week and the first half of the next week. In this study in other words days make a difference. A word of caution is needed here though. When you look at the variation in survival in each category one sees that while the means are statistically different the error bars show some overlap with the previous half week. At a population level we are able to say that for the average late 23 week infant survival is expected to be about 30% in this study and about 55% at 24 +0-3 days. What do you say to the individual parent though? I am not suggesting that this information is useless as it serves to provide us with an average estimate of outcome. It also is important I believe in that it suggests that dating on average is fairly accurate. Yes the dates may be off for an individual by 5 – 14 days but overall when you group everyone together when a pregnancy is dated it is reasonably accurate for the population.
Don’t become a slave to the number
The goal of this post is to remind everyone that while these numbers are important for looking at average outcomes they do not provide strict guidance for outcome at the individual level. For an individual, the prenatal history including maternal nutrition, receipt of antenatal steroids, timing of pregnancy dating and weight of the fetus are just some of the factors that may lead us to be more or less optimistic about the chances for a fetus. Any decisions to either pursue or forego treatment should be based on conversations with families taking into account all factors that are pertinent to the decision for that family. Age is just a number as people say and I worry that a graph such as the one above that is certainly interesting may be used by some to sway families one way or another based on whether the clock has turned past 12 AM. At 23 weeks 3 days and 23 hours do we really think that the patient is that much better off than at 24 weeks 4 days and 1 hour?
by All Things Neonatal | Jul 8, 2016 | education, residents, Uncategorized
These were the words spoken to me when I was a medical student doing an elective rotation in maternal fetal medicine at Mt. Sinai hospital in Toronto in 1997. Setting aside your surprise that I once wanted to be an Obstetrician (yes it’s true), I should put in context the situation that I heard this career changing advice. The service I was on was intense. Intense in the sense that some of the attendings were quite demanding and in their endless pursuit of excellence in care demanded a great deal from the medical students, residents and fellows around them. While I don’t remember the name of the fellow I was working with any longer, I do recall the verbal abuse she took on a daily basis likely from some misguided notion that since the attending had to endure such humiliation during training others should have to experience such joy themselves. After one such encounter, I had the opportunity to go for a coffee with my fellow and I took the opportunity to learn her coping mechanisms.
“Kill Them With Kindness”
You see this was no ordinary fellow. No matter how much verbal abuse was hurled her way she smiled at the attending and asked what she could do to resolve whatever shortcoming was pointed out to her. She never seemed upset (although on the inside I can’t imagine how she couldn’t) but kept her composure. When I asked her how she endured the daily grind all she said were those four words. I was very curious about this strategy. It seemed to me that she was enabling such behaviour and quite honestly in this era of medicine I have my doubts that the attending could get away with it. Having said that while it might not be so dramatic these days, it does happen but to a lesser degree. She explained to me that she believed that when you are consistently nice to someone even in the face of aggression they have no choice but to settle down. As she put it, staying angry in the face of someone who is smiling and thanking you sincerely for your input is difficult even for the most aggressive types. I suppose it is similar to a someone who is teasing you, stopping when they see they can’t get a rise out of you. I really took what she said to heart and built my career around this principle.
The Power of the Word Please
A funny thing happened today which really is what triggered this memory for me. One of our nurses chose to write a verbal order for me. She started the verbal order off with “please”. When I saw the start of the order I laughed and said that is the way I would have written it and she told me she knew as that is how I usually start my orders! It is sincere and not meant to be a trick but I think I owe it in part to that fellow from many years ago who taught me to “kill them with kindness”. My use of the word please which I realize now I use more often than not might seem odd but I think it sends a message of respect. An order should be followed but perhaps the word please is a way of saying “I realize you are busy but if you could do this I would appreciate it!” In the end we are a team and putting a little niceness into our daily routine can go a long way.
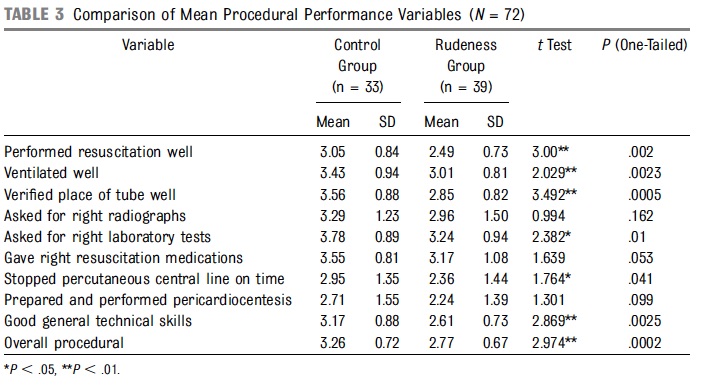
No Place For Rudeness
In a RCT designed to measure the impact of rudeness, medical teams were given a case to manage in a simulation exercise. The case was of a preterm infant now 23 days old with symptoms of NEC. Half the group met with a visitor who claimed to have observed such teams in their country before and in the rude environment made a disparaging comment about the past performance of the other teams. In the other group he simply mentioned he had observed other teams without commenting about their lack of skill. Simply planting the seed that previous performance of a similar team had been poor had damaging effects on team performance as shown below. Each item was rated from 1 = fail to 5 = excellent.
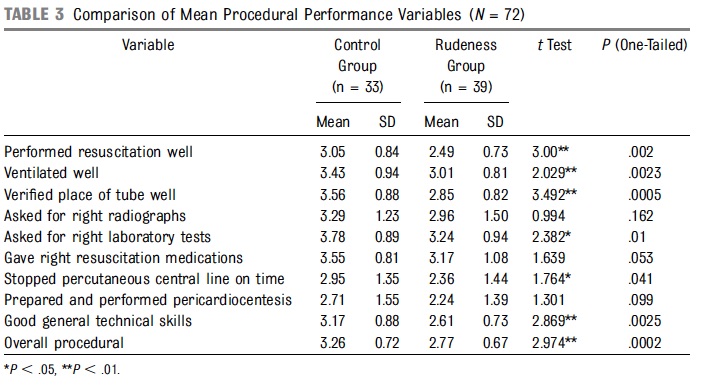
As you can see on many domains, team performance was impacted and in a significant way. Imagine how powerful more overt rudeness can be and damaging to the confidence and performance of the trainees and teams around you!
Let’s Get It Right
It’s July and that means there is a new crop of residents and fellows starting their journey towards becoming independent practitioners. This isn’t simulation anymore, this is the big leagues and they are working on real patients at risk of real adverse outcomes. Imagine if you will if the performance in the simulation above translated into poor performance in the hospital! We do our best to teach these “green” trainees the right way to do things but no amount of information will do them any good if we kill their confidence. Life as a new trainee is stressful enough. Can’t we all do a little to make things just a bit easier?
Yes it can be frustrating when they miss something important and yes that can have a consequence to patient care but if we want to minimize the greater risk to the patient population couldn’t we all do a little more to “Kill them with kindness” and say “please” from time to time?

by All Things Neonatal | Jul 7, 2016 | Uncategorized
After the recent CPS meeting I had a chance to meet with an Obstetrical colleague and old friend in Nova Scotia. It is easy to get lost in the beauty of the surroundings which we did. Hard to think about Neonatology when visits to places like Peggy’s Cove are possible.  Given out mutual interest though in newborns our our conversation eventually meandered along the subject of the new NRP. What impact would the new recommendations with respect to meconium have on the requirements for providers at a delivery. This question gave me reason to pause as I work in a level III centre and with that lens tend to have a very different perspective than those who work in level I and II centres (I know we don’t label them as such anymore but for many of you that has some meaning). Every delivery that is deemed high risk in our tertiary centre has ready access to those who can intubate so the changes in recommendations don’t really affect our staffing to any great degree. What if you are in a centre where the Pediatrician needs to be called in from home? Do you still have to call in people to prepare for a pending delivery of a baby through meconium stained fluid?
Given out mutual interest though in newborns our our conversation eventually meandered along the subject of the new NRP. What impact would the new recommendations with respect to meconium have on the requirements for providers at a delivery. This question gave me reason to pause as I work in a level III centre and with that lens tend to have a very different perspective than those who work in level I and II centres (I know we don’t label them as such anymore but for many of you that has some meaning). Every delivery that is deemed high risk in our tertiary centre has ready access to those who can intubate so the changes in recommendations don’t really affect our staffing to any great degree. What if you are in a centre where the Pediatrician needs to be called in from home? Do you still have to call in people to prepare for a pending delivery of a baby through meconium stained fluid?
What does the new recommendation actually say?
These recommendations are from the American Heart Association and are being adopted by the NRP committees in the US and Canada. The roll-out for this change is coming this fall with all courses required to teach the new requirements as of September 2017.
“However, if the infant born through meconium-stained amniotic fluid presents with poor muscle tone and inadequate breathing efforts, the initial steps of resuscitation should be completed under the radiant warmer. PPV should be initiated if the infant is not breathing or the heart rate is less than 100/min after the initial steps are completed. Routine intubation for tracheal suction in this setting is not suggested, because there is insufficient evidence to continue recommending this practice. (Class IIb, LOE C-LD)“
The rationale for the change is that is that there is a lack of evidence to demonstrate that routine suctioning will reduce the incidence of meconium aspiration syndrome and its consequences. Rather priority is placed on the establishment of adequate FRC and ventilation thereby placing a priority on teaching of proper bag-valve mask or t-piece resuscitator. Better to establish ventilation than delay while atempting to intubate and run the risk of further hypoxia and hypercarbia causing pulmonary hypertension.
Does this mean you don’t need to have a person skilled in intubation at such deliveries?
This question is the real reason for the post. At least from my standpoint the answer is that you do in fact still require such people. This may seem to be in conflict with the new position but if you move past that recommendation above you will see there is another line that follows afterwards that is the basis for my argument.
“Appropriate intervention to support ventilation and oxygenation should be initiated as indicated for each individual infant. This may include intubation and suction if the airway is obstructed.”
While we should not routinely perform such intubations there may be a time and a place. If one has intiated PPV with a mask and is not obtaining a rising heart rate, MRSOPA should be followed and attempts made to optimize ventilation. What if that is unsuccessful though and heart rate continues to be poor. You could have a plug of meconium distal to the vocal cords and this is the reason that intubation should be considered. In order to remove such a plug one would need to have an intubator present.
Where do we go from here?
As much as I would like to tell my colleague that he doesn’t need to have this skill set at a delivery for meconium I am afraid the skill still needs to be present. It will be interesting to see how instructors roll this out and answer such questions. It is a little concerning to me that in our world of wanting the “skinny” or “Coles’ Notes” version of things, the possibility of still needing the intubator on short notice may be lost. Having someone on call who is only “5 minutes away” may seem to be alright but at 3 AM I assure you the 5 minutes will become 15 as the person is woken, dresses, gets to the car and parks. Whether it is 5 or 15 minutes each centre needs to ask themselves if the baby is in need of urgent intubation are you willing to wait that amount of time for that to happen?
I hope not.



 You the reader might be more convinced of your actions but if I manipulate the numbers a little bit to say 105 g/l and HcT of 37% might you feel different? What about 110 g/L and 39%? You get the picture. Where is that magic cutoff where we say prior to an OR that a baby needs blood or can wait? In our heads of course we conjure up the equation for delivery of O2 to tissues Cardiac output X (1.39 X HgB X Sat +0.003*pO2) and realize that the delivery of oxygen is critically dependent on HgB level but how much is enough? The truth is I don’t think we really know but we do a good job of coming up with some markers such as lactate or more recently near infrared spectroscopy to give us an idea of how much O2 the tissues are seeing.
You the reader might be more convinced of your actions but if I manipulate the numbers a little bit to say 105 g/l and HcT of 37% might you feel different? What about 110 g/L and 39%? You get the picture. Where is that magic cutoff where we say prior to an OR that a baby needs blood or can wait? In our heads of course we conjure up the equation for delivery of O2 to tissues Cardiac output X (1.39 X HgB X Sat +0.003*pO2) and realize that the delivery of oxygen is critically dependent on HgB level but how much is enough? The truth is I don’t think we really know but we do a good job of coming up with some markers such as lactate or more recently near infrared spectroscopy to give us an idea of how much O2 the tissues are seeing.


 Given out mutual interest though in newborns our our conversation eventually meandered along the subject of the new NRP. What impact would the new recommendations with respect to meconium have on the requirements for providers at a delivery. This question gave me reason to pause as I work in a level III centre and with that lens tend to have a very different perspective than those who work in level I and II centres (I know we don’t label them as such anymore but for many of you that has some meaning). Every delivery that is deemed high risk in our tertiary centre has ready access to those who can intubate so the changes in recommendations don’t really affect our staffing to any great degree. What if you are in a centre where the Pediatrician needs to be called in from home? Do you still have to call in people to prepare for a pending delivery of a baby through meconium stained fluid?
Given out mutual interest though in newborns our our conversation eventually meandered along the subject of the new NRP. What impact would the new recommendations with respect to meconium have on the requirements for providers at a delivery. This question gave me reason to pause as I work in a level III centre and with that lens tend to have a very different perspective than those who work in level I and II centres (I know we don’t label them as such anymore but for many of you that has some meaning). Every delivery that is deemed high risk in our tertiary centre has ready access to those who can intubate so the changes in recommendations don’t really affect our staffing to any great degree. What if you are in a centre where the Pediatrician needs to be called in from home? Do you still have to call in people to prepare for a pending delivery of a baby through meconium stained fluid?