
by All Things Neonatal | Jun 30, 2016 | nutrition, Uncategorized
Breast milk has many benefits and seems to be in the health care news feeds almost daily. As the evidence mounts for long term effects of the infant microbiome, more and more centres are insisting on providing human milk to their smallest infants. Such provision significantly reduces the incidence of NEC, mortality and length of stay. There is a trade-off though in that donor milk after processing loses some of it’s benefits in terms of nutritional density. One such study demonstrated nutritional insufficiencies with 79% having a fat content < 4 g/dL, 56% having protein content< 1.5 g/dL, and 67% having an energy density < 67 kcal/dL (< 20 Kcal/oz). It is for this reason that at least in our unit many infants on donor milk ultimately receive a combination of high fluid volumes, added beneprotein or cow’s milk powders to achieve adequate caloric intake. Without such additions, growth failure ensues. Such growth failure is not without consequence and will be the topic of a future post. One significant concern however is that failure of our VLBW infants to grow will no doubt impact the timing of discharge as at least in our unit, babies less than 1700g are unlikely to be discharged. With the seemingly endless stream of babies banging on the doors of the NICU to occupy a bed, any practice that leads to increasing lengths of stay will no doubt slow discharge and cause a swelling daily patient census.
What if increasing volume was not an option?
Such might be the case with a baby diagnosed with BPD. Medical teams are often reluctant to increase volumes in these patients due to concerns of water retention increasing respiratory support and severity of the condition. While diuretics have not been shown to be of long term benefit to BPD they continue to be used at times perhaps due to old habits or anecdotal experiences by team members of a baby who seemed to benefit. Such use though is not without it’s complications as the need to monitor electrolytes means more needle sticks for these infants subjecting them to painful procedures that they truly don’t need. Alternatively, another approach is to restrict fluids but this may lead to hunger or create little room to add enough nutrition again potentially compromising the long term health of such infants.
Amy Hair and colleagues recently published the following study which takes a different approach to the problem Premature Infants 750–1,250 g Birth Weight Supplemented with a Novel Human Milk-Derived Cream Are Discharged Sooner
This paper is essentially a study within a study. Infants taking part in an RCT of Prolacta cream (Prolacta being the subject of a previous post) were randomized as well to a cream supplement vs no cream. The cream had a caloric density of 2.5 Kcal/mL and was added to donor milk or mother’s own milk when the measured caloric density was less than 19 Kcal/oz. The study was small (75 patients; control 37, cream 38) which should be stated upfront and as it was a secondary analysis of the parent study was not powered to detect a difference in length of stay but that was what was reported here. The results for the groups overall were demonstrated an impact in length of stay and discharge with the results shown below.
|
Control (N=37) |
Cream (N=38) |
p |
| PDA ligation % |
8.1 |
2.6 |
0.36 |
| PDA treated medically % |
27 |
29 |
0.85 |
| Sepsis % |
5.4 |
7.9 |
1 |
| NEC% |
0 |
0 |
– |
| BPD% |
32.4 |
23.7 |
0.4 |
| Death % |
0 |
0 |
– |
| Length of stay, days |
86+/-39 |
74+/-22 |
0.05 |
| PMA at discharge, weeks |
39.9+/-4.8 |
38.2+/-2.7 |
0.03 |
What about those with sensitivity to fluid?
Before we go into that let me state clearly that this group comparison is REALLY SMALL (control with BPD=12 vs cream with BPD=9). The results though are interesting.
|
BPD control (N=12) |
BPD cream N=9 |
p |
| Length of stay, days |
121 +/-49 |
104+/-23 |
0.08 |
| PMA at discharge, weeks |
44.2+/-6.1 |
41.3+/-2.7 |
0.08 |
So they did not reach statistical significance yet one can’t help but wonder what would have happened if the study had been larger or better yet the study was a prospective RCT examining the use of cream as a main outcome. That of course is what no doubt will come with time. I can’t help but think though that the results have biologic plausibility. Providing better nutrition should lead to better growth, enhanced tissue repair and with it earlier readiness for discharge.
One interesting point here is that the method that was used to calculate the caloric density of milk was found to overestimate the density by an average of 1.2 Kcal/oz when the method was compared to a gold standard. Given that fortification with cream was only to be used if the caloric density of the milk fell below 19 Kcal/oz where average milk caloric density is 20 Kcal/oz there is the distinct possibility that the eligible infants for cream were underestimated. Could some of the BPD be attributable to infants being significantly undernourished in the control group as they actually were receiving <19 Kcal/oz but not fortified? Could the added fortification have led to faster recovery from BPD?
Interesting question’s in need of answers. I look forward to seeing where this goes. I suspect that donor milk is not enough, adding a little cream may be needed for some infants especially those who have trouble tolerating cow’s milk fortification.

by All Things Neonatal | Jun 23, 2016 | Parents, Uncategorized
A good idea that is for sure and stress may be what the infant in the picture is displaying as a reflection of what her parents are feeling! A growing trend is to include parents in rounds and that is the subject of this piece? It sounds like a great idea and may feel that way as you have had a personal experience that has been favourable, is the practice in your unit or it just seems to make sense? It might come as a surprise to you who have followed this blog for some time that I would even ask the question but a social media friend of mine Stefan Johansson who runs 99NICU sent an article my way on this topic. Having participated in the FiCare study I realised that I have a bias in this area but was intrigued by the title of the paper. The study is Parental presence on neonatal intensive care unit clinical bedside rounds: randomised trial and focus group discussion by Abdel-Latif ME et al from New Zealand and was performed due to the lack of any RCTs on the subject specifically in the NICU.
Before I go on though I have to disclose a few biases.
- I love parents being on rounds so I can speak with them directly and have them ask me any questions they may have after hearing about their infants condition.
- Our unit encourages the practice.
- We are rolling out the principles of FiCare after being part of the study which encourages parental presence at the bedside for far more than just rounds.For information on implementing FiCare click here
- While this study is the only reported RCT on the subject in the NICU, the FiCare results will be published before long.
What is the problem with having families on rounds?
The detractors would say that sensitive information may be more difficult to discuss out in the open for fear that the family will take offence or be hurt. Another concern may be that teaching will be affected as the attending may not want to discuss certain aspects of care in order to prevent creating fear in the parents or awkwardness in the event that the management overnight was not what they would have done. Lastly, when patient volumes and acuity are high, having parents ask questions on rounds may lead to excessive duration of this process and lead to fatigue and frustration by all members of the team.
So what does this study add?
This particular study enrolled 72 families of which 63 completed the study. The study required 60 families to have enough power to detect the difference in having parents on rounds or not.The design was interesting in that the randomisation was a cross over design in which the following applied. One arm was having parents on rounds and the other without. The unit standard at the time was to not have parents on rounds.
≤30 weeks 1 week in one arm, one week washout period then one week in the other arm
>30 weeks 3 days in one arm, three day washout and then three days in the other arm
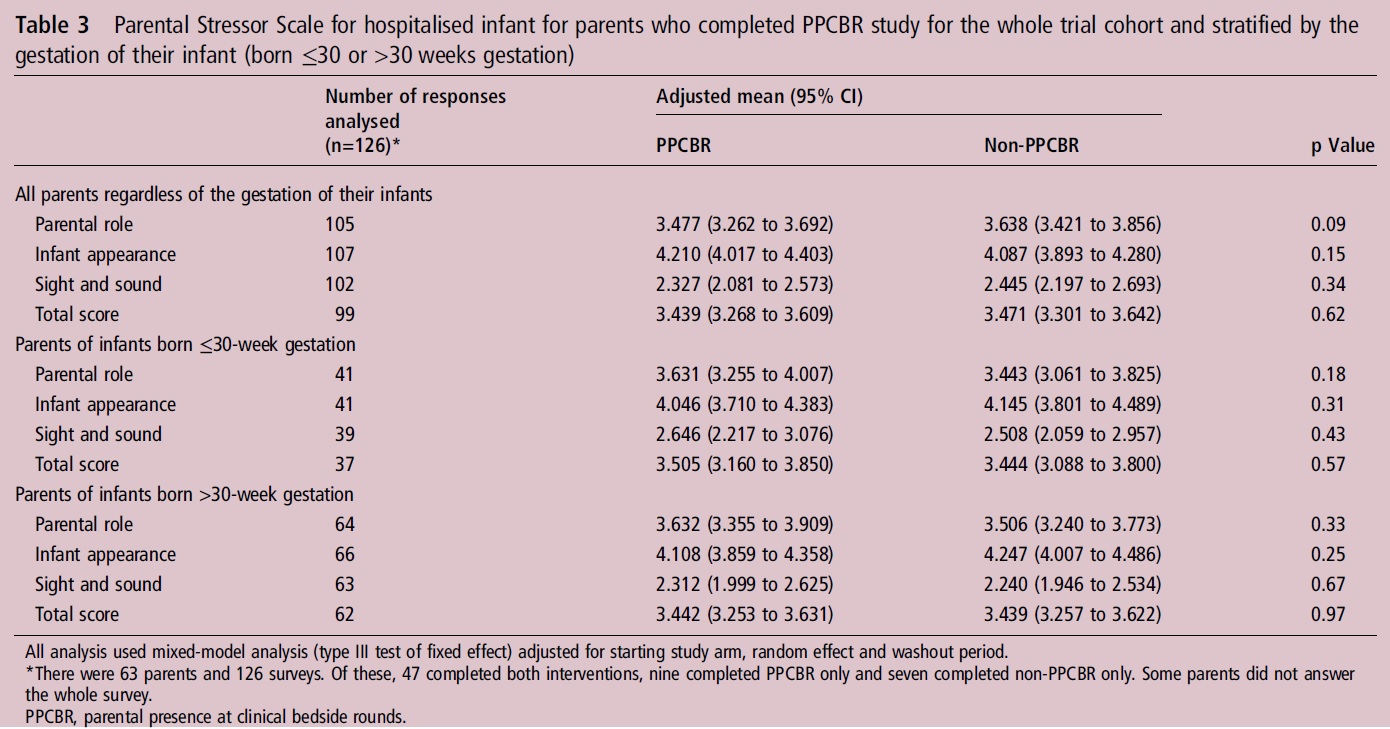
The primary outcome was to see if there would be a significant difference in the Parental Stressor Scale. 
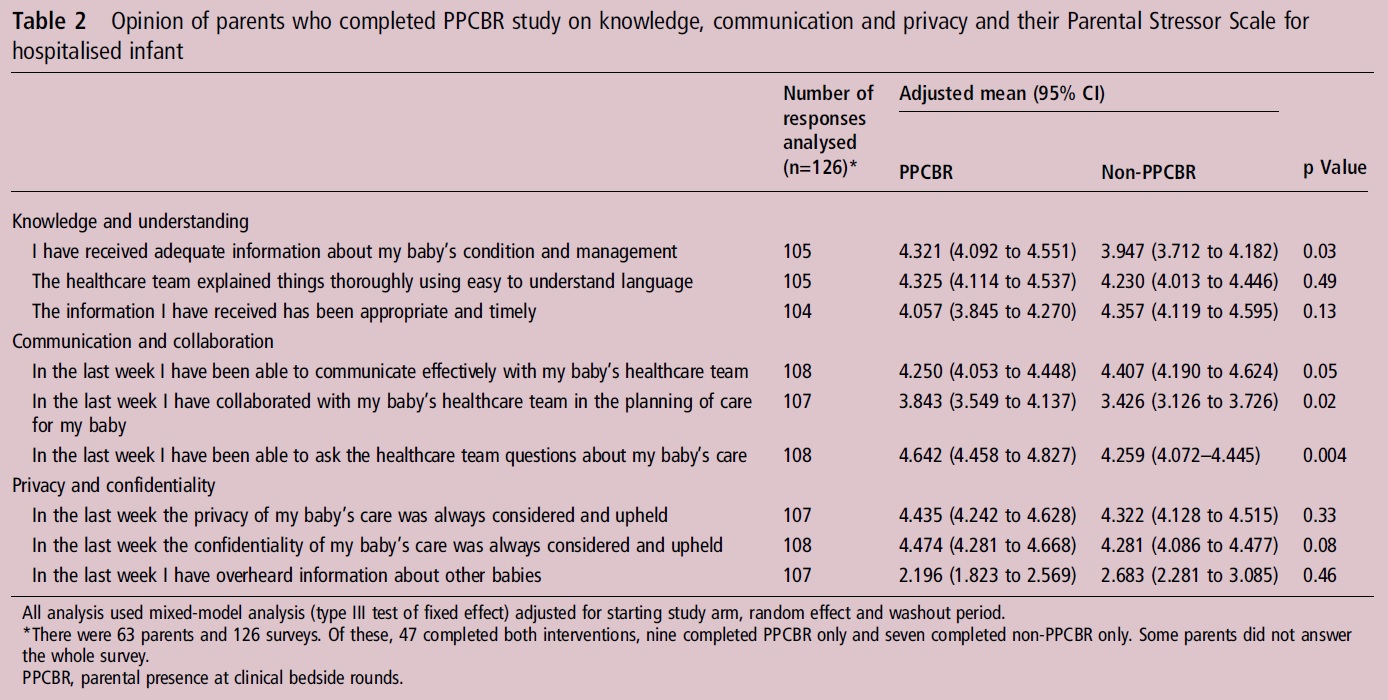
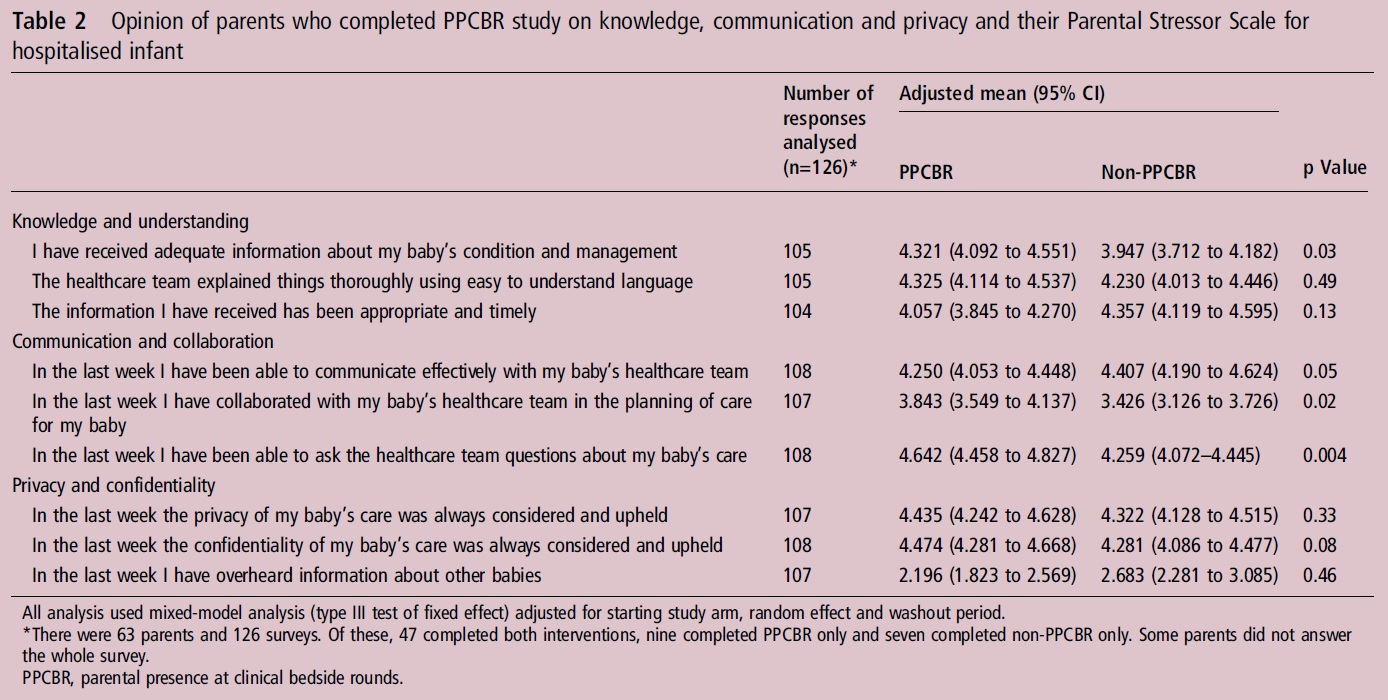
Surprisingly there was no difference across any domains of measuring parental stress. When we look at questions though pertaining to communication in the NICU we see some striking differences.
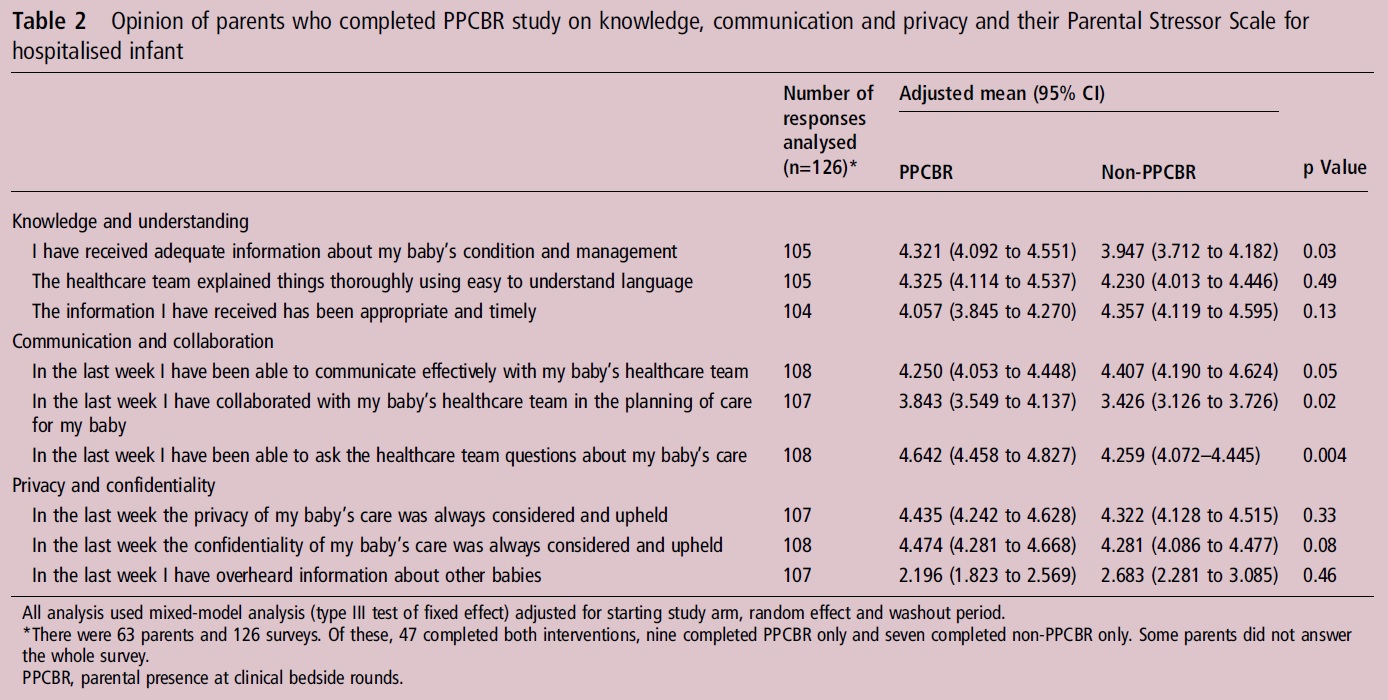
The families see many benefits to the model of being on rounds. They appear to have received more information, more contact with the team, contributed more to the planning of the course of their babies care and been able to ask more questions. All of these things would seem to achieve the goals of having parents on rounds.
So why aren’t parents less stressed?
This to me is the most interesting part of this post. The short answer is I am not sure but I have a few ideas.
- The study could not be blinded. If the standard of care in the unit was to not have parents on rounds, what kind of conversations happened after rounds? Were staff supportive of the families or were they using language that had a glass is half empty feel to it? Much like I am biased towards having parents on rounds and thanking them for their participation were there any negative comments that may have been unintentional thrown the families way.
- Is a little knowledge a dangerous thing? Perhaps as families learn more details about the care of their baby it gives them more things to worry about. Could the increase in knowledge while in some ways being pleasing to the family be offset by the concern that new questions raise.
- Was the intervention simply too short to detect a difference? This may have been a very important contributor. This short period of either a week or two leaves the study open to a significant risk that an event in either week could acutely increase stress levels. What if the infant had to go back on a ventilator after failing CPAP, needed to be reloaded with caffeine or developed NEC? With such short intervals one cannot say that while communication was better the parents were not stressed due to something unrelated to communication. In an RCT these should balance out but in such a small study I see this as a significant risk.
So where do we go from here?
I applaud the authors for trying to objectively determine the effect of parental presence on rounds in the NICU. Although I think they did an admirable job I believe the longer time frame of the FiCare study and the cluster randomised strategy using many Canadian centres will prove to be the better model to determine effectiveness. What the study does highlight though in a very positive way is that communication is enhanced by having parents on rounds and to me that is a goal that is well worth the extra time that it may take to get through rounds. Looking at it another way, we as the Neonatologists may need to spend less time discussing matters after rounds as we have taken care of it already. In the end it may be the most efficient model around!

by All Things Neonatal | Jun 23, 2016 | Parents, Uncategorized
To many of you the answer is a resounding yes in that it reduces stress. Why is that though? Is it because you have had a personal experience that has been favourable, it is the practice in your unit or it just seems to make sense? It might come as a surprise to you who have followed this blog for some time that I would even ask the question but a social media friend of mine Stefan Johansson who runs 99NICU sent an article my way on this topic. Having participated in the FiCare study I realised that I have a bias in this area but was intrigued by the title of the paper. The study is Parental presence on neonatal intensive care unit clinical bedside rounds: randomised trial and focus group discussion by Abdel-Latif ME et al from New Zealand and was performed due to the lack of any RCTs on the subject specifically in the NICU.
Before I go on though I have to disclose a few biases.
- I love parents being on rounds so I can speak with them directly and have them ask me any questions they may have after hearing about their infants condition.
- Our unit encourages the practice.
- We are rolling out the principles of FiCare after being part of the study which encourages parental presence at the bedside for far more than just rounds.For information on implementing FiCare click here
- While this study is the only reported RCT on the subject in the NICU, the FiCare results will be published before long.
What is the problem with having families on rounds?
The detractors would say that sensitive information may be more difficult to discuss out in the open for fear that the family will take offence or be hurt. Another concern may be that teaching will be affected as the attending may not want to discuss certain aspects of care in order to prevent creating fear in the parents or awkwardness in the event that the management overnight was not what they would have done. Lastly, when patient volumes and acuity are high, having parents ask questions on rounds may lead to excessive duration of this process and lead to fatigue and frustration by all members of the team.
So what does this study add?
This particular study enrolled 72 families of which 63 completed the study. The study required 60 families to have enough power to detect the difference in having parents on rounds or not.The design was interesting in that the randomisation was a cross over design in which the following applied. One arm was having parents on rounds and the other without. The unit standard at the time was to not have parents on rounds.
≤30 weeks 1 week in one arm, one week washout period then one week in the other arm
>30 weeks 3 days in one arm, three day washout and then three days in the other arm
The primary outcome was to see if there would be a significant difference in the Parental Stressor Scale. 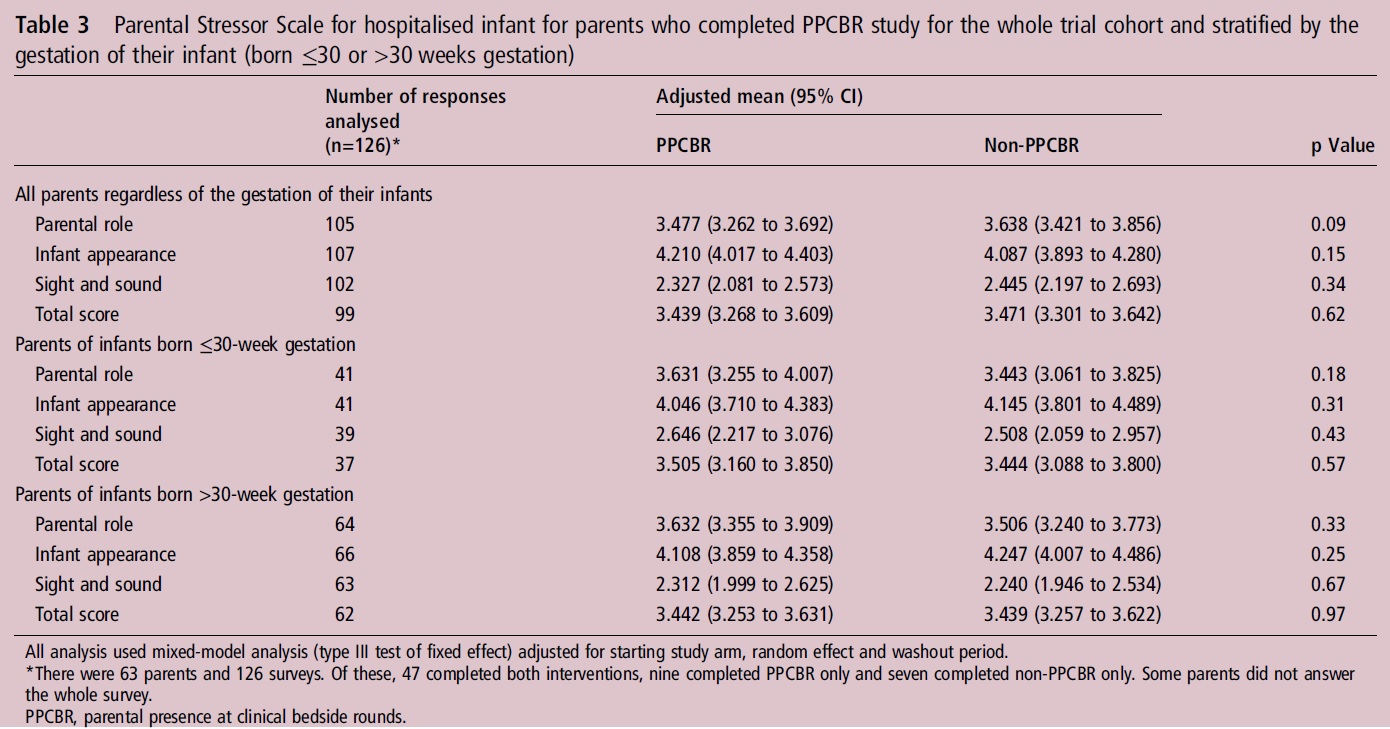
Surprisingly there was no difference across any domains of measuring parental stress. When we look at questions though pertaining to communication in the NICU we see some striking differences.
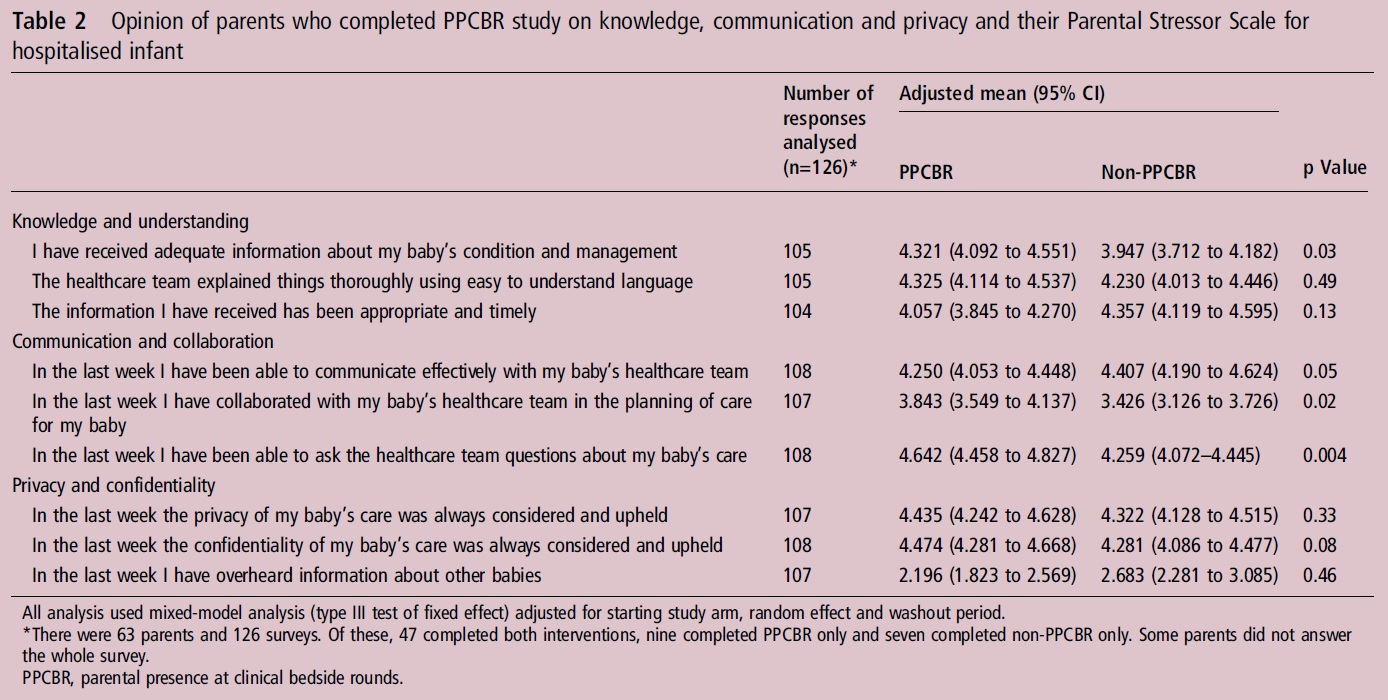
The families see many benefits to the model of being on rounds. They appear to have received more information, more contact with the team, contributed more to the planning of the course of their babies care and been able to ask more questions. All of these things would seem to achieve the goals of having parents on rounds.
So why aren’t parents less stressed?
This to me is the most interesting part of this post. The short answer is I am not sure but I have a few ideas.
- The study could not be blinded. If the standard of care in the unit was to not have parents on rounds, what kind of conversations happened after rounds? Were staff supportive of the families or were they using language that had a glass is half empty feel to it? Much like I am biased towards having parents on rounds and thanking them for their participation were there any negative comments that may have been unintentional thrown the families way.
- Is a little knowledge a dangerous thing? Perhaps as families learn more details about the care of their baby it gives them more things to worry about. Could the increase in knowledge while in some ways being pleasing to the family be offset by the concern that new questions raise.
- Was the intervention simply too short to detect a difference? This may have been a very important contributor. This short period of either a week or two leaves the study open to a significant risk that an event in either week could acutely increase stress levels. What if the infant had to go back on a ventilator after failing CPAP, needed to be reloaded with caffeine or developed NEC? With such short intervals one cannot say that while communication was better the parents were not stressed due to something unrelated to communication. In an RCT these should balance out but in such a small study I see this as a significant risk.
So where do we go from here?
I applaud the authors for trying to objectively determine the effect of parental presence on rounds in the NICU. Although I think they did an admirable job I believe the longer time frame of the FiCare study and the cluster randomised strategy using many Canadian centres will prove to be the better model to determine effectiveness. What the study does highlight though in a very positive way is that communication is enhanced by having parents on rounds and to me that is a goal that is well worth the extra time that it may take to get through rounds. Looking at it another way, we as the Neonatologists may need to spend less time discussing matters after rounds as we have taken care of it already. In the end it may be the most efficient model around!

by All Things Neonatal | Jun 15, 2016 | Uncategorized, ventilation
As the saying goes the devil is in the details. For some years now many centres worldwide have been publishing trials pertaining to high flow nasal cannulae (HFNC) particularly as a weaning strategy for extubation. The appeal is no doubt partly in the simplicity of the system and the perception that it is less invasive than CPAP. Add to this that many centres have found less nasal breakdown with the implementation of HFNC as standard care and you can see where the popularity for this device has come from.
This year a contact of mine Dominic Wilkinson on twitter (if you don’t follow him I would advise having a look!) published the following cochrane review, High flow nasal cannula for respiratory support in preterm infants. The review as with most cochrane systematic reviews is complete and comes to a variety of important conclusions based on 6 studies including 934 infants comparing use of HFNC to CPAP.
1. No differences in the primary outcomes of death (typical RR 0.77, 95% CI 0.43 to 1.36; 5 studies, 896 infants) or CLD.
2. After extubation to HFNC no difference in the rate of treatment failure (typical RR 1.21, 95% CI 0.95 to 1.55; 5 studies, 786 infants) or reintubation (typical RR 0.91, 95% CI 0.68 to 1.20; 6 studies, 934 infants).
3. Infants randomised to HFNC had reduced nasal trauma (typical RR 0.64, 95% CI 0.51 to 0.79; typical risk difference (RD) -0.14, 95% CI -0.20 to -0.08; 4 studies, 645 infants).
4. Small reduction in the rate of pneumothorax (typical RR 0.35, 95% CI 0.11 to 1.06; typical RD -0.02, 95% CI -0.03 to -0.00; 5 studies 896 infants) in infants treated with HFNC but the RR crosses one so this may be a trend at best.
If one was to do a quick search for the evidence and found this review with these findings it would be very tempting to jump on the bandwagon. Looking at the review a little closer though there is one line that I hope many do not miss and I was happy to see Dominic include it.
“Subgroup analysis found no difference in the rate of the primary outcomes between HFNC and CPAP in preterm infants in different gestational age subgroups, though there were only small numbers of extremely preterm and late preterm infants.”
In his conclusion he further states:
Further evidence is also required for evaluating the safety and efficacy of HFNC in extremely preterm and mildly preterm subgroups, and for comparing different HFNC devices.
With so few ELBW infants included and with these infants being at highest risk of mortality and BPD our centre has been reluctant to adopt this mode of respiratory support in the absence of solid evidence that it is equally effective to CPAP in these smallest infants. A big thank you to our Respiratory Therapy Clinical Specialist for harping on this point over the years as the temptation to adopt has been strong as other centres turn to this strategy.
Might Not Be So Safe After All
Now do not take what I am about to say as a slight against my twitter friend. The evidence to date points to exactly what he and his other coauthors concluded but with the release of an important paper in May by Taka DK et al, I believe caution is needed when it comes to our ELBW infants.
High Flow Nasal Cannula Use Is Associated with Increased Morbidity and Length of Hospitalization in Extremely Low Birth Weight Infants
This paper adds to the body of literature on the topic as it truly focuses on the outcome of infants < 1000g. While this study is retrospective in nature it does cover a five year period and examines important outcomes of interest to this population.
The primary outcome in this case was death or BPD and whether HFNC was used alone or with CPAP, this was more frequent than when CPAP was used alone. Other important findings were the need for multiple and longer courses of ventilation in those who received at least some HFNC. In these times of overburdened health care systems with goals of improving patient flow, it is also worth noting that there was a significant prolongation of length of stay with use of HFNC or HFNC and CPAP.
One interesting observation was that the group that fared the worst across the board was the combination of CPAP and HFNC rather than HFNC alone.
|
CPAP (941) |
HFNC (333) |
HFNC +/- CPAP (1546) |
| CPAP d (median, IQR) |
15(5-28) |
|
7 (1-19) |
| HFNC d (median, IQR) |
14(5-25) |
13 (6-23) |
| HFNC +/- CPAP |
15 (5-28) |
14(5-25) |
26 (14-39) |
| BPD or death % |
50.40% |
56.80% |
61.50% |
| BPD % |
42.20% |
52.20% |
59.00% |
| Multiple ventiation courses |
51.10% |
53.10% |
64.70% |
| More than 3 vent courses |
17.60% |
21.00% |
29.40% |
| Ventilator d (median, IQR) |
18(5-42) |
25 (6-52) |
30 (10-58) |
I believe the finding may be explained by the problem inherent with retrospective studies. This is not a study in which patients were randomized to either CPAP, HFNC or CPAP w/HFNC. If that were the case one would expect lung pathologies and severity of illness to even ou,t such that differences between groups might be explained by the difference in treatments. In this study though we are looking though the rearview mirror so to speak. How could we account for the combination being worse than the HFNC alone? I suspect it relates to the severity of lung disease. The babies who were placed on HFNC and did well on it might have had less severe chronic changes. What might be said about those that had the combination? Well, one could postulate that there might be some who were extubated to HFNC and collapsed needing escalation to CPAP and then failing that therapy were reintubated. Another explanation could be those babies who were placed on CPAP after extubation and transitioned before their lungs were ready to HFNC may have failed and lost FRC thereby going back to CPAP and possibly intubation. Exposure in either circumstance to HFNC would therefore put them at risk of further positive pressure ventilation and subsequent further lung injury. The babies who could tolerate transition to HFNC without CPAP might be intermediary in their outcomes (as they were found to be) as they lost FRC but were able to tolerate it but consumed more calories leaving less for growth and repair of damaged tissue leading to prolonged need for support.
Either way, the use of HFNC was found to lead to worse outcomes and in the ELBW infant should be avoided as routine practice pending the results of a prospective RCT on the subject.
Is it a total ban though?
As with many treatments that one should not consider standard of care there may be some situations where there may be benefit. The ELBW infant with nasal breakdown from CPAP that despite excellent nursing and RRT attention continues to demonstrate tissue damage is one patient that could be considered. The cosmetic implications and potential for surgical correction at a later date would be one reason to consider a trial of HFNC but only in the patient that was close to being able to come off CPAP. In the end I believe that if a ELBW infant needs non invasive pressure support then it should be with CPAP but as there saying goes there may be a right time and a place for even this modality.

by All Things Neonatal | Jun 1, 2016 | technology, Uncategorized
When you mention electronic medical records to some physicians you get mixed responses. Some love them and some…well not so much. These tech heavy platforms promise to streamline workflows and reduce error with drop down menus, some degree of artificial intelligence in providing warnings when you stray too far from acceptable practice but for some who are not so tech savvy they are more of a pain. I have to admit I am in the camp of believing they are a good thing for patient care as I work in one centre with expanded EMR services and one without and I do find a number of benefits to working with a more robust EMR platform but I respect that not all do.
The cell phone on the other hand is everywhere and even the most tech fearful often carry one including most of the parents we care for. What caught my eye this month was the article by Globus O The use of short message services (SMS) to provide medical updating to parents in the NICU in which an EMR system is described that sends parents a text message at a pre-specified time regarding their infants condition. I had a visceral reaction at first thought thinking “would I want my cell phone number sent to families?”, “how much time out of the day would all of this take?” and to be a little old fashioned “can’t we just talk on the phone?”. I am sure there are many other questions that others would have as well. Having said that as I read through the paper I warmed to the concept and by the end questioned whether we could do the same!
The Intervention
It turns out the SMS message comes from the EMR and not the personal cell phone of the bedside nurse and is sent out at 9 AM each day. Each nurse requires only 30 seconds of their day to populate a few questions during the night shift and then the information goes out to the parents.
“The text message includes one-sentence prefaces and conclusions and provides updated information that includes the location of the infant’s crib (room and position), the infant’s current weight and whether medical procedures, such as head ultrasound, cardiac echocardiogram or eye examination, were performed. Information regarding acute events or deterioration of the infant’s medical condition are not included in the SMS, but are delivered personally to the parents in real time.”
This last sentence is important. The SMS service will not notify the family that their infant is receiving chest compressions but is there to give them “updates”. The sceptics out there will likely comment that this should be the job of both nursing and medicine to regularly update the families but thinking about it, how many parents are not there everyday and when they are out of sight how many physicians regularly call them to provide them updates? No doubt there are some but I would think they are not in the majority.
But is it effective?
The measurement in this case was through surveys of nursing and families both pre-implementation and afterwards. Provided in the table below are the scores (means +/- SD) in the pre and post implementation phases of the program.
| Statement |
Pre-SMSi N=91 |
Post SMSi N=87 |
P-value |
| The physician was available when needed |
4.1+/-0.9 |
4.4+/-0.7 |
0.002 |
| The physician was patient in answering my questions |
4.6+/-0.7 |
4.9 +/-0.4 |
0.002 |
| I felt comfortable approaching the physicians |
4.3+/-1.0 |
4.7+/-0.6 |
0.001 |
| I felt comfortable approaching the nurses |
4.4+/-0.8 |
4.6+/-0.6 |
0.02 |
| I regularly received information from the physicians regarding my infant’s medical status |
3.7+/-1.3 |
4.1+/-1.1 |
0.03 |
These are some pretty powerful outcomes. The use of what many consider an impersonal form of communication (how many times have I looked at people texting furiously and thought JUST PICK UP THE PHONE!) actually appears to have improved the approachability of the staff in the unit and facilitated information transfer more easily.
One other important finding was that when surveyed pre-intervention staff were somewhat sceptical that this would help and moreover were concerned that it would interfere too much with work flow in the day. Evaluations afterwards did not support these fears and many felt it was an improvement. In the end the total time spent on this by nursing was estimated to be no more than 30 seconds of each day! From the parent’s standpoint they certainly saw this as an improvement.
The Future
At least in our centre we are moving slowly but steadily towards a fully functioning EMR. Will we have this capability in the software that we use? After reading this I hope so. I can see how receiving a daily morning message would prime the family to interact with staff on rounds. The added benefit is that by knowing that the information would be ready at 9 AM, families could be present with questions already formulated in their minds. How often do we encourage families to be on rounds and have them listen to a tremendous amount of information and then turn to them with the standard “any questions?”. While I am sure many of us try and explain matters in lay terms, giving parents a change to mull over the issues first could well enhance the interaction they have with our team in a meaningful way.
Time to look into whether this is possible…

by All Things Neonatal | May 26, 2016 | Uncategorized
We have been seemingly under siege over the last year or so by a relentless flow of preterm infants through our units in the city. Peaks and valleys for patient census come and go for the most part but this almost unwavering tendency to be filled to the rafters so to speak is unusual. Much has been said and will continue to be acknowledged that we are all doing incredible work, that we are dedicated and putting patients first but where is the breaking point? When does fatigue lead to errors no matter how well intentioned and selfless we are. In those cases when it is not a matter of being selfless but we are mandated to come in fatigue is no less an issue.
Like many units in North America and in other parts of the world, rates of neonatal sepsis have been on the decline but during a recent peak in both acuity and volume in the region we saw a spike in the rate of culture proven sepsis. At a time when we were at our busiest our sepsis rate worsened which raised many eyebrows as to what could be contributing. It is tempting to blame it on patient volumes but what is the actual evidence to support such a claim. This is the thrust of this piece and I hope you find the topic of some relevance to you as we continue on this journey of a higher state of patient volumes in the city.
Nurse to Patient Ratio is Likely Important
This has to be important right?! NICUs come in many shapes and sizes but if you can staff appropriately with 1:1, 1:2 and 1:3 ratios based on patient acuity if you had enough nurses would your sepsis rates be ok? To answer this a useful study is by Jeannie P. Cimiott et al entitled Impact of staffing on bloodstream infections in the neonatal intensive care unit. The study group was actually from an RCT on hand hygiene and this study was a reanalysis of the data to determine for infants with confirmed sepsis what impact nursing hours had in the context of a patient with their first positive blood culture. In her study there were 2675 infants in two New York level III NICUs that had 224 positive blood cultures. The impact of nursing hours on risk of infection was dramatic.
The NICU with greater nursing coverage had a significantly decreased risk (HR, 0.21; 95% CI, 0.06-0.79) of bloodstream infection. Moreover, the more RN hours per nursing intensity weight was associated with a 79% reduction in the risk of bloodstream infection in the unit with greater nursing work hours. 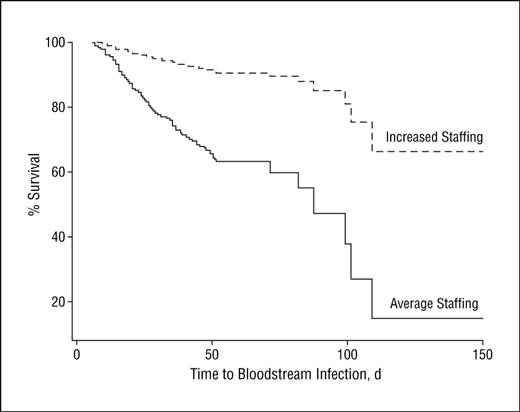 Looking also at the impact of greater nursing hours on time to infection demonstrated the following curve. From the graph one can see that two patients both of which develop an infection at 100 days of life have markedly different chances of survival based on the staffing level. The Neonatologist, RRT, dietician could all be the same but if the nursing hours are lacking the patient is more likely to die. A very significant concern indeed!
Looking also at the impact of greater nursing hours on time to infection demonstrated the following curve. From the graph one can see that two patients both of which develop an infection at 100 days of life have markedly different chances of survival based on the staffing level. The Neonatologist, RRT, dietician could all be the same but if the nursing hours are lacking the patient is more likely to die. A very significant concern indeed!
What Effect Does The Percentage of Preterm Babies In The Unit Have On The Rate of Infections?
The next question may be answered by looking at a study from this year by Goldstein et al entitled Characteristics of late-onset sepsis in the NICU: does occupancy impact risk of infection? This study looked retrospectively at a 17 year period between 1997 and 2014 to determine the risk of systemic infection from two standpoints; occupancy and percentage of infants < 32 weeks. In other words they were looking at whether the presence of many smaller babies in the units increases such risk of infection specifically. This was a rather large study population of 19810 infants of which 446 had confirmed late onset sepsis. Not surprisingly 70% of the cases of sepsis were with CONS.
The authors examined hazard ratios to determine whether occupancy or proportion of infants < 32 weeks had an effect on risk and determined that the average occupancy did not correlate with risk of infection but did for the category of infants < 32 weeks. Interestingly the HR for this was 1.03 with a CI that touches 1 so I am not sure how they make this claim but in the end they conclude:
“For each additional percentage of infants <32 weeks gestation in the unit, neonates had an increased late-onset sepsis hazard of 2% (HR 1.02, 95% CI: 1.00, 1.03) over their NICU hospitalization.”
For arguments sake let’s say this is a real effect. I do have to call into question the diagnosis of sepsis. I could not find mention of the definition of sepsis in this cohort and with so many CONS infections I do worry that some of these were in fact contaminants. Did they draw one or two blood cultures in each instance? How many of these if they had would have had one positive and the other negative? Having just a few of these labelled as contaminants may have negated any effect seen.
What About The Nurses?
You also can’t ignore the fact that while they looked at occupancy they made no attempt to control for the amount of staff. To not do so I think misses a very important point. Whether your unit is functioning at 60, 70, 80 or more occupancy while giving a measure of patient volumes tells you nothing about the coverage for such patients. In a well staffed unit with adequate nurse to patient ratios there might be minimal risk of error. If assignments though that are ideally 2:1 are stretched to 3 or 4: 1 that is likely where the errors start to come in.
Coming back to our situation that likely mirrors many other centres across the globe I believe all of this comes down to ensuring a safe environment to care for our patients. A safe environment means having enough staff to cover the number of patients and that includes medical, RRTs, dieticians and others. The message from all of this is that to do our best we need the right amount of staff to do it. We can handle the volume, just provide us with the resources to handle it. If it is money that we are hoping to save consider the amount of dollars that could be saved by avoiding prolonged stays from infection and all the associated morbidities that follow.
Then there is the increase in mortality to consider and I for one will not even begin to put a price on that.







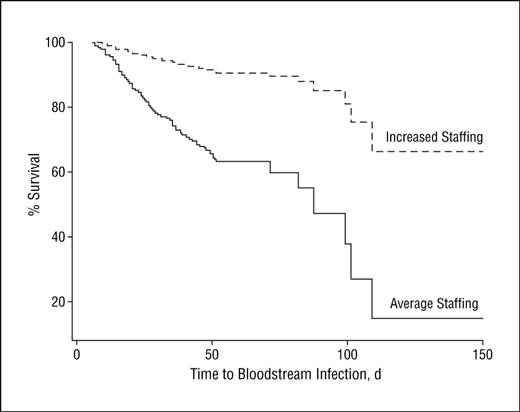 Looking also at the impact of greater nursing hours on time to infection demonstrated the following curve. From the graph one can see that two patients both of which develop an infection at 100 days of life have markedly different chances of survival based on the staffing level. The Neonatologist, RRT, dietician could all be the same but if the nursing hours are lacking the patient is more likely to die. A very significant concern indeed!
Looking also at the impact of greater nursing hours on time to infection demonstrated the following curve. From the graph one can see that two patients both of which develop an infection at 100 days of life have markedly different chances of survival based on the staffing level. The Neonatologist, RRT, dietician could all be the same but if the nursing hours are lacking the patient is more likely to die. A very significant concern indeed!