The story is typical. A family notices a small red spot in the weeks following delivery which enlarges over the next month. They present to their family doctor or Pediatrician who identifies the most common skin lesion in childhood; a hemangioma affecting about 3-10% of all children depending on the population observed. As a resident I was given the following advice regarding hemangiomas; “As long as the hemangioma is not of cosmetic concern, sight threatening, multiple in number or causing anemia or thrombocytopenia watchful waiting is recommended.” Furthermore I recall the following general advice that while they tend to enlarge over the first year of life, 40% are gone by 4 years, 60% by 6 years and 90% by 9 years. After my training I started a practice passing along the same advice to the infants I now cared for.
Then something happened similar to the serendipitous discovery of penicillin. In 2008, Leaute-Labreze et al published a case report in which they described a child being treated for a facial hemangioma with corticosteroids. Unfortunately the hemangioma did not respond to treatment but rather led to a cardiomyopathy requiring treatment with propranolol. Curiously the hemangioma demonstrated significant regression on propranolol. The results of this case report prompted further treatments with propranolol in an unblinded fashion. Since this time propranolol and more recently topical Timolol (sample size 41) have been studied both in observational and small randomized controlled trials. Propranolol while effective has potential side effects such as hypotension, bradycardia and bronchospasm which has limited it’s widespread application except for those patients with either large, sight threatening or multiple hemangiomas. Topical timolol in the RCT above was demonstrated to be safe and when given locally, free of such side effects making it a seemingly ideal treatment for smaller hemangiomas that may have some cosmetic concerns later in life as they regress. That being said, the time of onset for regression was noted to be after 12-16 weeks of therapy and the target they aimed for was a reduction of >5% which is certainly modest. While only a small improvement it was seen 60% of the time in the treatment group and 11% in the placebo arm. From personal experience I have used topical Timolol with patients in the NICU with varying success but in some cases the results were quite impressive. Looking at the RCT by Chan, timolol was only applied to those hemangiomas that were small and deemed unsuitable for treatment with propranolol.
This leaves us with the question; what does one use if anything for larger hemangiomas which traditionally don’t fit into the category of needing treatment vs patient observation. Secondly, is it wise to systematically treat all larger hemangiomas with propranolol as outpatients, given the potential severity of the side effects, some of which may be life threatening.
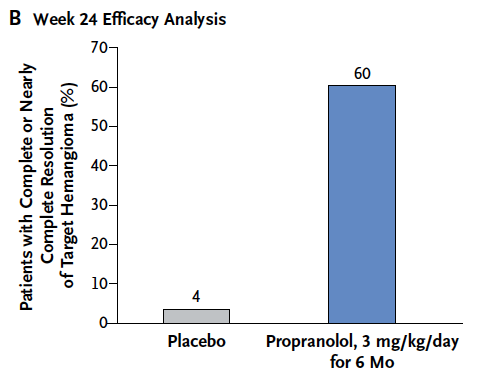
This past week in the New England Journal of Medicine we have come full circle as Leaute-Labreze et all have published a large prospective RCT http://bit.ly/1ACqn2C to determine the optimal dose and duration of propranolol for treatment of hemangiomas requiring systemic treatment. The number of patients enrolled in this study was 456 which makes it the largest study to date in this field. This study sought to determine whether 1 mg/kg/day vs 3 mg/kg/day divided twice a day for 3 or 6 months would provide the best resolution without unacceptable side effects. Eligible patients were between 1-5 months of age with a proliferating hemangioma and were treated for either 3 or 6 months depending on which arm of the study they were on. The results of this trial were striking and found that the best balance of benefit and risk was with 3 mg/kg/day for 6 months and is shown below graphically compared to placebo.
This difference translates into a number need to treat to cause regression = 1.7 or rounded up 2. For every two patients that you treat with propranolol you will cause one hemangioma to regress. Try finding a therapeutic benefit like that in another trial!
But what about safety? Side effects were rare compared to placebo but not negligible. The most common side effect was diarrhea and with respect to life threatening adverse effects the only one really noted was bradycardia but in a patient with enterocolitis. My take on this treatment is that it appears to have great impact with little downside!
How do we apply these results though to “real life” situations. We now have as I see it a “one-two punch”. Hemangiomas that are deemed to require no systemic treatment can be treated with a safe topical drop that has been used for years for glaucoma patients. Patients with larger more significant hemangiomas may be treated with a highly efficacious treatment that may have very few side effects.
The downside of systemic therapy at least in Winnipeg is that treatment with propranolol generally requires a hospital admission at the start of treatment to monitor for side effects that would be considered life threatening. With an incidence of 5% of children it would be impractical to admit 600 children a year for such treatment based on an estimated 12000 births in the region a year.
I do believe the time is upon us for change though. As I see it, gone are the days where we tell parents that we will see what develops when their child has a small hemangioma. If you have a willing parent who is concerned about the hemangioma and it is < 1.5 cm in size I believe topical Timolol should be offered to the family for a period of 6 months treatment. Anything larger than that would merit treatment with propranolol. Nine years is potentially a very long time to wait for a lesion to regress and potentially leave a scar or telangiectasia behind. If we can do something about it now with such a high rate of success and minimal risk to the patient, why wait?
My advice to you if you either have a child with a hemangioma or know someone else with one is to have them ask their doctor whether Timolol or Propranolol would be right for them. Given these findings I know my practice will change.

Une hospitalisation de quelques heures suffit pour monitorer la tension artérielle.
Ils repartent avec une fiche conseil en cas de gastro ou bronchite.
Bien prendre pendant le repas avoir une alimentation régulière.
Qu l angiome gêné par le regard des autre ou intervient sur le regard des parents pourquoi pas?
Je crois aussi un court séjour à assurer la stabilité serait raisonnable .
Pardonnez mon français que je ai dû utiliser Google Translate !
Hi i think its a great comment. And in prematures this is a very common problem. Thanks for traslate stadistics to us. Sorry for my english I am spanish speaker from mexico
Your English is more than fine. My Spanish would be much worse. Thank you for the comment and I hope the blog is helpful to you and others. Much more to come! If you or others wish to get automatic updates via email just click on the purple follow button on the right side of the blog
Thanks for putting this together Michael, I look forward to reading your blog. Wish we could work together again, you are such a great teacher!
All the best from Kelowna!
Jason
Glad you like it. Miss seeing your face around here
Thank you for your Intresting blog.
Hemangioma found in infants is benign tumour, normally a self-involuting tumor in the form of swelling or extra growth of the endothelial cells that lines the blood vessels. It is characterized as increase in total number of normal or abnormal blood vessels.
http://www.orchidlaser.com/
Thank you.
I’m surprised this article and research no mention of PHACE syndrome. Any child with a large or segemental hemangioma should be evaluated for PHACE syndrome per guidelines.
Many thanks, excellent effort & with simplified & detailed discussion, thank you again.