As the saying goes, sometimes less is more. In recent years there has been a move towards this in NICUs as the benefits of family centred care have been shown time and time again. Hi tech and new pharmaceutical products continue to develop but getting back to the basics of skin to skin care for many hours and presence of families as an integral team member have become promoted for their benefits. The fetus is a captive audience and hears the mother’s heart beat and voice after the development of hearing sometime between 24-26 weeks gestational age. This is a normal part of development so it would stand to reason that there could be a benefit to hearing this voice especially after hearing has developed and the fetus has grown accustomed to it. Hospital including my own have developed reading programs for our patients and some companies have developed speakers in isolettes designed to limit the maximum decibel to 45 but allowing parents to make recordings of their voices. Music may be played through these speakers as well but today we will focus on the benefit of voice.
Could reading to your baby reduce apnea of prematurity?
This is the question that Scala M et al sought to answer in their paper Effect of reading to preterm infants on measures of cardiorespiratory stability in the neonatal intensive care unit. This was a small prospective study of the impact of parental reading on cardiorespiratory stability in preterm NICU infants. Eighteen patients were enrolled who were born between 23-31 weeks gestation. The study was carried out when the babies were between 8-56 days old at a mean postnatal age of 30 weeks. Each patient served as their own control by comparing episodes of oxygen desaturation to <85% during pre-reading periods (3 hours and 1 hour before) to during reading and then 1 hour post reading. Parents were asked to read or create a recording lasting a minimum of 15 min but up to 60 min of recorded reading. The parents were offered a standard set of books that had a certain rhythm to the text or could choose their own. Recorded reading was played for infants up to twice per day by the bedside nurse. While it was small in number of patients the authors point out that the total exposure was large with 1934 min of parental bedside reading analyzed (range 30–270 min per infant, mean 123, median 94 min). Patients could be on respiratory support ranging from ventilators to nasal cannulae.
Was it effective?
It certainly was. I should mention though that the authors excluded one patient in the end when it was found that they failed their hearing screen.  Arguably, since the infant could not have benefited from the intervention effect this makes sense to me. As shown from table 3 there was a statistical reduction in desaturation events during the reading period which was sustained in terms of a downward trend for one hour after the intervention was completed.
Arguably, since the infant could not have benefited from the intervention effect this makes sense to me. As shown from table 3 there was a statistical reduction in desaturation events during the reading period which was sustained in terms of a downward trend for one hour after the intervention was completed. 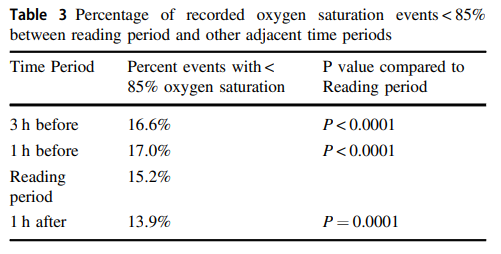 In case you are asking was the difference related to oxygen use the answer is no. There was no difference in the amount of oxygen provided to patients. While the events were not eliminated they were certainly reduced. The other point worth mentioning is that there appears to be a difference between live (through open portholes) vs prerecorded reading (through a speaker in the isolette).
In case you are asking was the difference related to oxygen use the answer is no. There was no difference in the amount of oxygen provided to patients. While the events were not eliminated they were certainly reduced. The other point worth mentioning is that there appears to be a difference between live (through open portholes) vs prerecorded reading (through a speaker in the isolette).
Now for a little controversy
Does source of the reading matter? The authors found that maternal had a greater effect than paternal voice.  As a father who has read countless books to his children I found this a little off-putting. As a more objective critic though I suppose I can buy the biologic plausibility here. I suspect there is an independent effect of voice having a positive impact on development. If we buy the argument though that the voice that the fetus has most been accustomed to is the mothers, then the findings of an augmented effect of the maternal voice over fathers makes some sense. I will have to put my ego aside for a moment and acknowledge that the effect here could be real.
As a father who has read countless books to his children I found this a little off-putting. As a more objective critic though I suppose I can buy the biologic plausibility here. I suspect there is an independent effect of voice having a positive impact on development. If we buy the argument though that the voice that the fetus has most been accustomed to is the mothers, then the findings of an augmented effect of the maternal voice over fathers makes some sense. I will have to put my ego aside for a moment and acknowledge that the effect here could be real.
There will no doubt need to be larger studies done to drill down a number of questions such as what is the ideal type of reading, duration, rhythmic or non etc but this is a great start. I also think this falls into the category of “could this really be a bad thing?”. Even if in the end no benefit is shown to this type of intervention, the potential for family bonding with their preterm infant alone I think is cause for embracing this intervention.
Lastly, with the move to single patient rooms there is one study that demonstrated the isolation encountered from infrequent contact with their newborn can have a long lasting effect on development. The article by Pineda RG et al Alterations in brain structure and neurodevelopmental outcome in preterm infants hospitalized in different neonatal intensive care unit environments. had a mean parental visitation of 19 +/- 19 hours a week or a little over 2 hours a day but with a very large standard deviation meaning many infants had almost no visitation. The message here is that while quiet is good for infant development, too much can be a bad thing. Maybe live reading or even recordings are a way around that.