Anyone who works in the NICU is more than familiar with the sad moment when you find out an infant has suffered a severe IVH (either grade III or IV) and the disclosure to the family. The family is in a state of shock with the fear of ventricular drainage a reality that will likely come to pass. We have spent many years trying to find ways to reduce this risk and antenatal steroids and delayed cord clamping are two relatively recent interventions that have had a real impact. Unfortunately we have not been able to eliminate this problem though. What if something as simple as an exclusive human milk diet could be that magic bullet to further reduce this problem in our NICUs?
Exclusive human milk diets
I have written about this topic before but as a refresher this generally refers to all sources of nutrition being derived from human milk. Ideally we would provide mothers own milk (MOM) but when this is not available units rely on pasteurized donor human milk (PDHM) as the base feed. Added to this is human derived human milk fortifier (H2HMF) as opposed to bovine powdered or liquid fortifier usually to provide a base caloric density of 24 cal/oz.
Reducing IVH Through Exclusive Human Milk Diets
It would be nice to have a prospective multicentre trial with this as the outcome but there is a significant problem when doing this type of study. The H2HMF is costly with a price tag of about $13-15000 per treatment course so to do a prospective RCT would not be easy for units that don’t use the product already. Moreover, for those units that are already sold on the product it would seem unethical if there was no equipoise to randomize to bovine or human fortifier. As such, when we talk about getting the best evidence it is most likely going to come in the form of a retrospective study as has been done here by Carome K et al in their paper Exclusive human milk diet reduces incidence of severe intraventricular hemorrhage in extremely low birth weight infants.
The authors in this study chose to look at three different time periods with different approaches to feeding of ELBW infants. They were as follows with all diets providing H2HMF going until 34 weeks. Aside from the source of nutrition, starting of and incremental advancement of feedings was protocolized as per unit approach.
2012 to 2014 – MOM was given when available. Preterm formula was the alternative as a supplement Fortification of was with bovine milk-derived liquid fortifier
2014 to 2015 – H2HMF used in those infants receiving exclusively MOM. All others received preterm formula as supplement or alternative. If MOM was available but in insufficient quantities for sole diet, it was fortified with bovine-HMF
2015 to 2017 – all ELBW infants received an EHM diet consisting of MOM if available and PDHM as a supplement to MOM or as full diet, each fortified with H2HMF
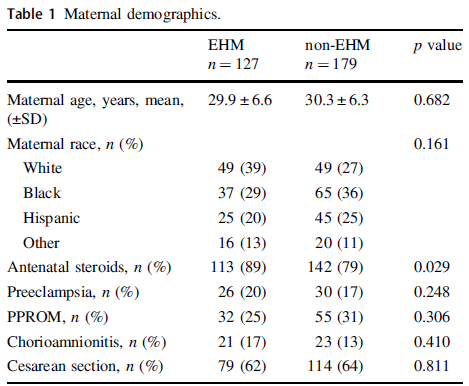
The maternal demographics were similar between those receiving exclusive human milk diets and those without except for a higher antenatal steroid provision in the EHM group. This of course bears consideration in the results as steroids have been shown to reduce IVH.
Looking at the results below shows some very promising findings. The incidence of Grade III/IV IVH and/or PVL was 7% in the EHM group and 18% in the non-EHM group. Also noted to be quite different was the incidence of NEC which was 5% in the EHM and 17% in the non group. The authors also did a subgroup analysis looking at the use of MOM vs PDHM and found no difference in outcomes regardless of source of human milk used. As the authors point out this might mean that the pasteurization process does not denature the components of milk responsible for these protective effects if the results are to be believed.
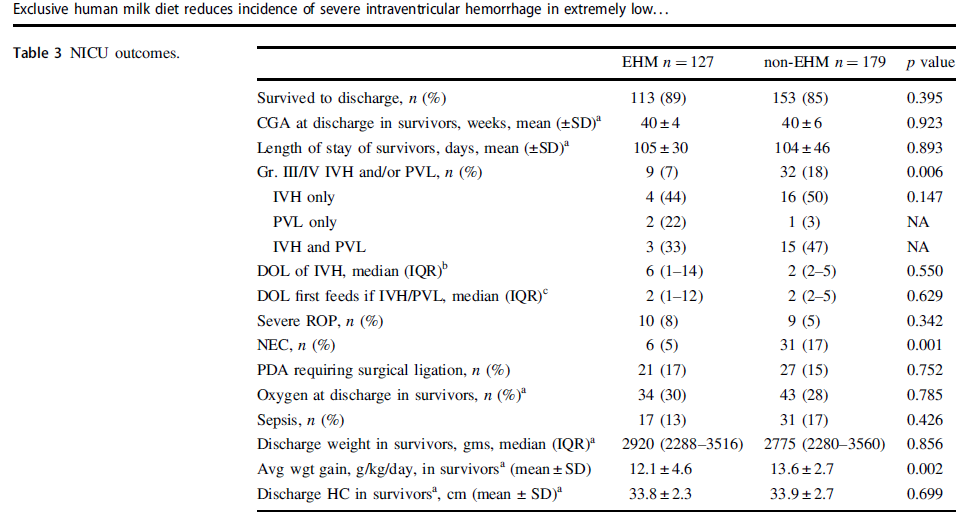
One strength of the study was that the authors performed a logistic regression to control for the higher rate of antenatal steroid use and lower rates of NEC in the EHM group since both would be expected to influence rates of IVH/PVL and found that the results remained significant after this analysis. The findings were an OR of 2.7 CI 1.2–6.0, p = 0.012 so that is promising!
What They Weren’t Able to Do
It’s possible I missed it in the article but like several other papers on this topic the babies who received formula and those who received human milk with bovine fortifier were grouped together. As such what we don’t know from this study is whether the addition of just the bovine fortifier vs H2HMF would have yielded the same results.
Nonetheless what the article does suggest is that use of EHM diets are protective against severe IVH/PVL regardless of the source of human milk when you compare it to receipt of any bovine sources. The caveats about retrospective studies of course exist as per usual but if this is the best evidence we have how do we use it? At the very least this calls out for strategies to maximize milk production for mothers and to use PDHM when MOM is not available. It certainly is suggestive that the use of H2HMF may confer benefit as well. What you unit does with this information I suppose will need to be determined based on the totality of the evidence. I suspect there is more of this story to be told and this adds yet another chapter in the tale of EHM.


Seems like the incidence of severe IVH is quite high in the non-EHM group when we look at our data and VON data. The timing of bleeds in relation to onset and volume of feedings and other possible management changes over time needs to be considered. But yes, for many reasons MOM is best.
Completely agree that MOM is best. This study does seem to have quite a few challenges when it relates to protection against something that occurs before most patients ever get colostrum. The use of vasopressors to maintain blood pressure especially in the transition period is not mentioned. And over the course of 5 years, a lot has changed in resuscitation and care of newborn that is not ingrained in unit policy. Anyways, this is a work product that we should continue to support. Great work Scientist!