With American Thanksgiving coming up this weekend a post about “cold turkey” seemed apropos. You can’t work in Neonatology and not be familiar with CPAP. We have learned much about this modality in the last couple decades as clinicians have moved more and more towards non-invasive support as the preferred strategy for supporting newborns regardless of gestational age. Ask a Neonatologist how they use CPAP and you will find varied opinions about how high to go and how quickly to wean. I have written about one weaning strategy before on this blog using monitor oxygen saturation histogram data to make such decisions Improve your success rate in weaning from CPAP. One question though that has often been asked is what level of CPAP is best to remove a baby from? In particular for our smallest infants who may have BPD or reduced pulmonary reserve due to lower numbers of alveoli as they continue to develop should you discontinue at +5, +4 or +3? This question is what some creative authors from Texas sought to answer in the paper being discussed today.
To Wean or Not To Wean?
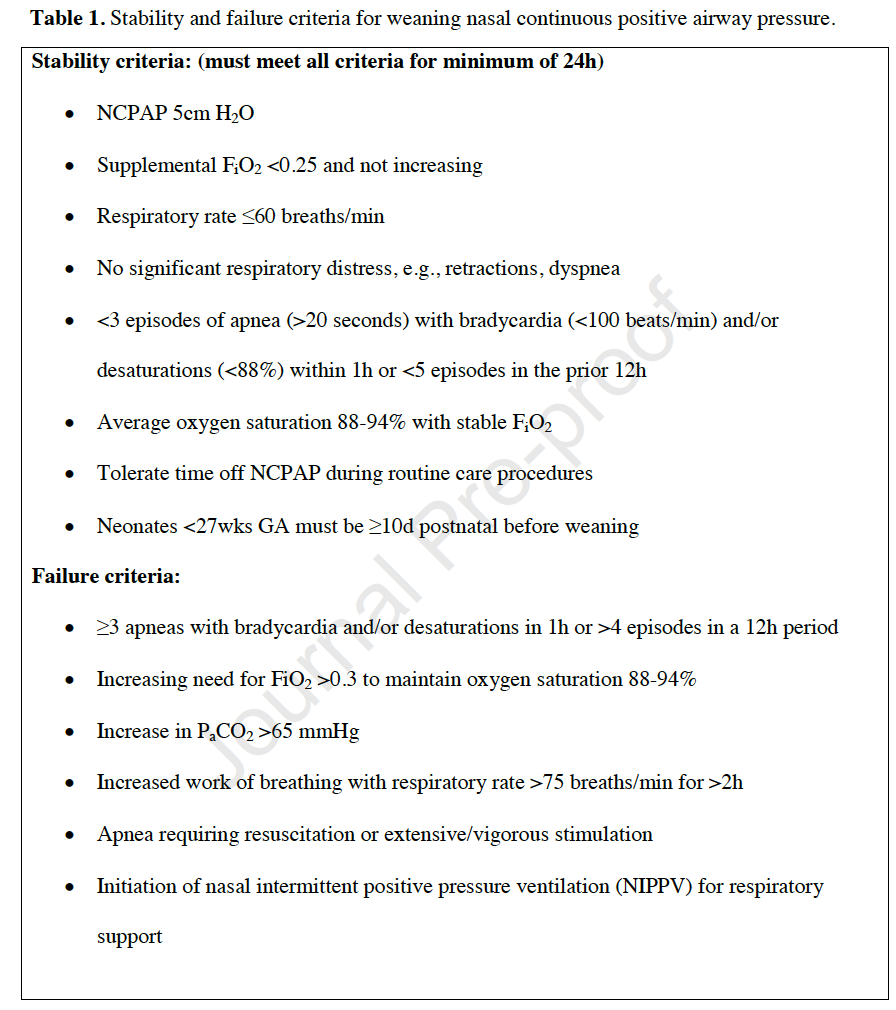
Kakkilaya V et al published Discontinuing Nasal Continuous Positive Airway Pressure in Infants ≤32 Weeks Gestational Age: A Randomized Control Trial in the Journal of Pediatrics this October. The authors studied infants from 23+0 to 32+6 weeks gestational age at birth and looked at whether a strategy of discontinuing from +5 or weaning from +5 to +3 then stopping resulted in fewer failures from stoppage. Infants were recruited in two ways. Some infants were intubated with planned extubation to pressures from +5 to +8 while others were on CPAP always. The study included 226 infants or which 116 were assigned to control so had removal of CPAP at +5 if after 24 hours they met the stability criteria below. The other 110 infants reduced CPAP from +5 once every 24 hours if the same criteria were met. Reasons for restarting CPAP were also as shown below at the bottom of Table 1. If an infant failed then they went back to the level of CPAP they had been on previously when stability criteria were met. Once they had stability criteria at that level again for 24 hours the wean could resume.
Did they manage to find a difference?
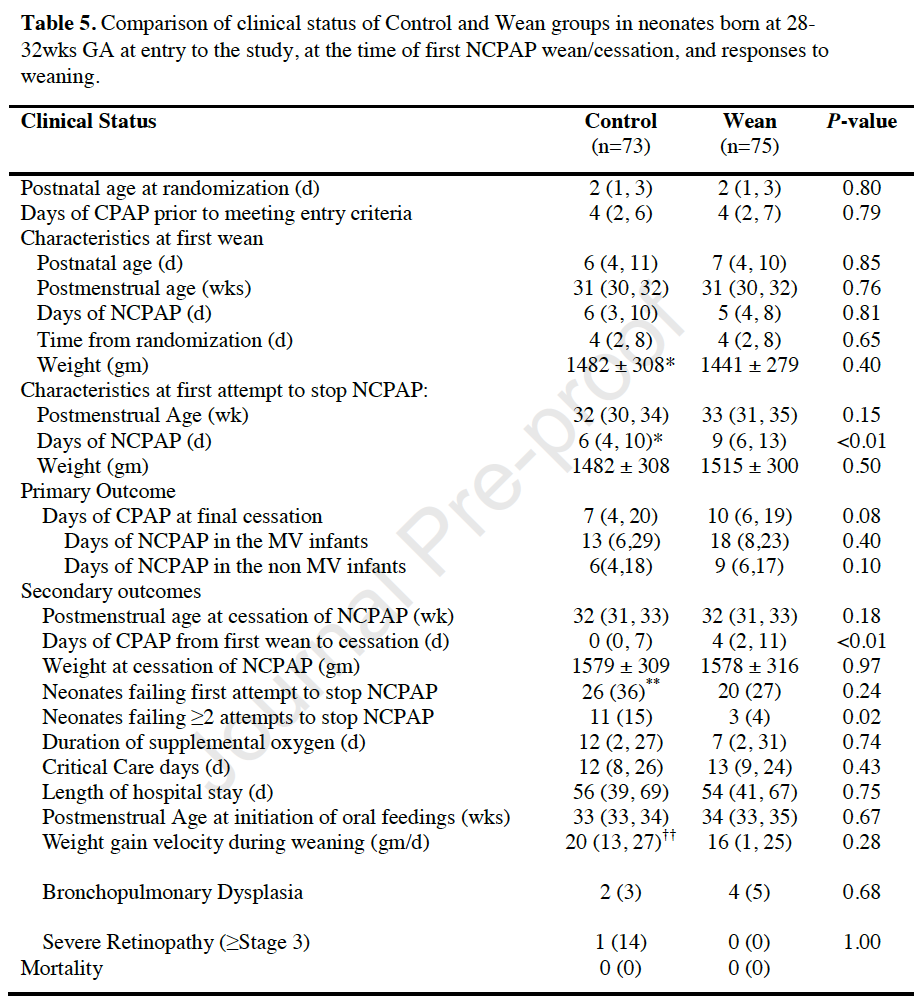
Table 5 reveals the significant finding here which is that for the primary outcome there was no difference and it didn’t matter whether the infants were ventilated or not. One finding that was different was the number of neonates who failed to stop CPAP two or more times. This favoured the weaning approach. Aside from that the groups were comparable and there really wasn’t much benefit seen from one approach versus the other.
Thoughts About the Study
The study was a fairly straightforward one and although there wasn’t a significant result found there are some questions that I think we can think about.
- The stability criteria did not have results from histogram analysis included as a measure of stability. I can’t help but wonder if addition of this approach would have identified some infants who were actually not ready to wean. Having said that, one challenge is to come to an agreement on what a stable histogram is. Based on a survey from my own colleagues recently I would say like many things in Neonatology, we are all over the map. If this study were to be repeated using histograms for decisions on weaning some sort of agreement would be needed on what qualifies as a stable histogram.
- Our group has already tended to use +4 as the final weaning step for our ELBW and VLBW infants based on anecdotal experience that many of these kids if stopped at +5 will fail even when they seem to be stable. Repeating this study looking at weaning from +4 to +3 before stopping vs stopping at +4 could be interesting as well.
- Finally, I do wonder if the wean was too fast to show a difference. It is not uncommon practice in the smallest infants to keep them on +4 for a couple days even if it seems that the histograms would indicate the baby is ready to stop CPAP. Perhaps a weaning strategy of allowing a minimum of q48h instead of q24h would have found different results?
I do think the authors explored a great question and I would be reluctant here to “throw the baby out with the bathwater”. There is something here but based on the methodology (which I don’t think is flawed per se) I think they just couldn’t prove what I suspect is true.

