I have written a lot over the years on the topic of BPD. It isn’t by chance as it is a condition that Neonatologists have put a lot of weight on. In many ways it is a benchmark that is often the go to condition when comparing one unit to another. When two Neonatologists get together their first question isn’t what’s your rate of ROP or severe developmental delay but more often comparing rates of BPD. We like to compare this as a metric as it’s something we can see as compared to say rates of late onset sepsis. You can see a patient on a ventilator or on CPAP at 36 weeks but you can’t see bacteria coursing through veins.
Not all BPD is the same though. in 2000 the NIH produced a new consensus definition of BPD as shown below.
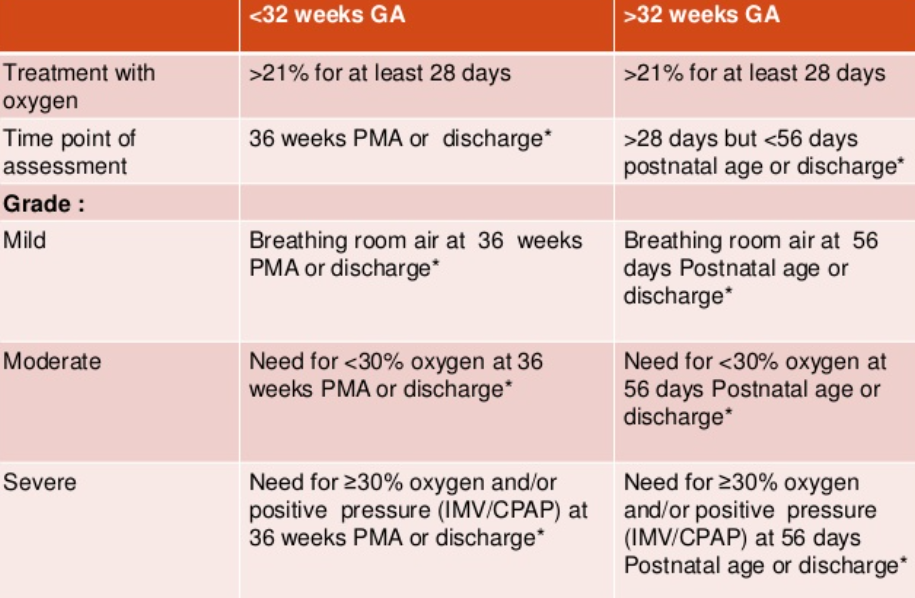
What stands out for the babies <32 weeks is how severe BPD is defined. Babies who are ventilated are classified in the same severity group as those who are on CPAP. Somehow that doesn’t seem quite right intuitively but alas that is what they decided at the time.
Thinking of a New Stratification
Guaman MC et al published Invasive mechanical ventilation at 36 weeks post-menstrual age, adverse outcomes with a comparison of recent definitions of bronchopulmonary dysplasia. The authors subdivided the severe category the following way:
Type 1 sBPD: patients on nasal cannula or noninvasive positive pressure support (i.e., high flow nasal cannula (HFNC), nasal continuous positive airway pressure (nCPAP), noninvasive intermittent positive pressure ventilation (nIPPV)) Type 2 sBPD: infants receiving iMV
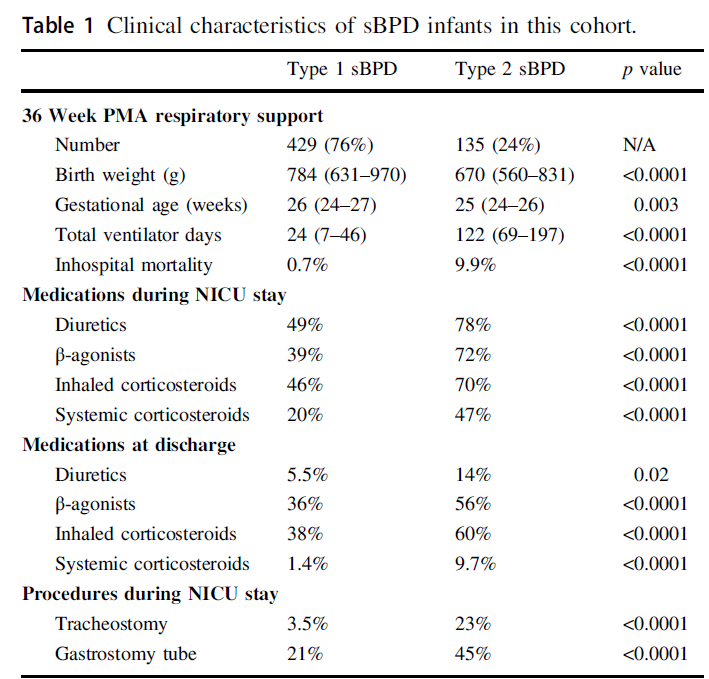
The authors then looked at a sample of 564 patients from 2015-2019 in the BPD collaborative registry and subdivided them into 429 (76%) Type 1 vs 135 (24%) Type 2 sBPD and compared outcomes between the two. The differences between the two types of BPD are quite significant and shown in Table I. Babies who went on to develop sBPD as Type 2 were younger and smaller than those with Type 1. Medication use within the NICU and after discharge was markedly different as were the total ventilator days which is likely not surprising since by definition they were still intubated at 36 weeks. Importantly if you were still intubated at 36 weeks PMA almost one quarter of the patients went on to receive a tracheostomy.
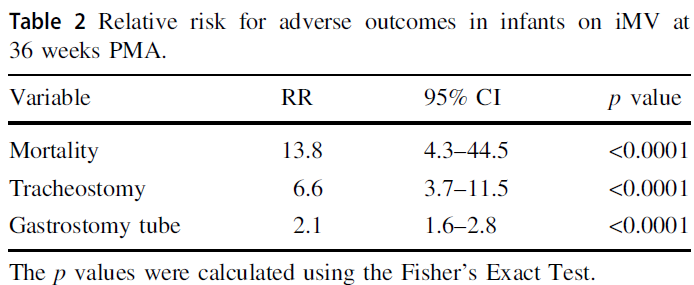
Looking at it another way using relative risks the signifance of having Type 2 sBPD is impactful.
Taking Meaning From This
You might be quick to say, Michael this is absolutely no surprise. On the other hand if you have read this blog for some time you may remember this piece The New BPD That Matters. This study looked at what gestational age really mattered when looking at long term pulmonary outcomes in a Canadian cohort. When you take all comers it was 40 weeks and not 36 weeks that really mattered. The likely differernce here though is that by selecting out only the severe patients in this current study it is indeed the 36 week mark that still has relevance. I actually think the two papers together are not contradictory but rather additive.
What I think one takes away from the current study is that failure to extubate by 36 weeks does in fact carry with it significant long term risk to the patient. It would be easy enough to say that these babies should be extubated but as you see from table I it isn’t that they didn’t try. From a medication standpoint it would appear that they ” threw the kitchen sink” at these babies. The only thing I find a little surprising is that only 47% of babies in the collaborative with type 2 sBPD received systemic steroids. If they were that sick I would have expected it to be higher although that also may just be a reflection of my own practice.
One thing that I think will be a hot topic moving forward is the use of higher levels of CPAP than what many units are accustomed to. This has also been recently discussed in High CPAP vs NIPPV. Is there a winner? There may be a reluctance by some units to use CPAP levels in the +9-12 cm H2O range but when looking at these downstream complications for patients who remain ventilated at 36 weeks I think people need to seriously consider their biases and whether they are based on science or what they were taught. I can’t help but think of the oft used expression absence of evidence is not evidence of absence and think that if we can all be a little humble who knows what we may discover that can help this population.

I’m very stunished by this results: 24% prémies still intubated and ventilated at 36.
Certainly in Europe we are not the champions of 24 weeks but this pourcentage is very high .Perhaps the americans teams should try LISA and ventilation in volume guaranted.And also sistemic corticotherapy earlier like 14-20 days in order to extubate those babys.
This is my opinion: I found those results very bad and I dont think that the prematurity is the only explications.