Jaundice has to be one of the most common issues facing newborns and their families. Whether in the NICU or on the post-partum floor all babies get jaundiced to a certain degree and some become so much so that they require treatment. Many centers the world over have developed home phototherapy programs to allow treatment to be done at home and they are known to be effective. In Sweden such programs exist and in theory sending infants home rather than keeping them in hospital could have positive effects for both the infant and parent dyad in terms of bonding. Keeping the infants in hospital and in particular over the last couple years when in many places of the world COVID protocols made visiting more difficult there is the real potential to disrupt bonding if a baby is otherwise ready for discharge. Researchers in Sweden with such programs in Uppsala recently decided to explore this question about bonding so here we go.
The Study
This was a multicentre study in Sweden by Pettersson M et al entitled Home phototherapy of term neonates improves parental bonding and stress: findings from a randomised controlled trial. The study intended to enroll 250 infant-parent pairs into an RCT comparing in-hospital phototherapy to home phototherapy and determine the status of bonding between child and parents at various time points. The inclusion criteria required infants to be >36 weeks at birth, have non-immune jaundice (DAT -ve) and have a bilirubin at inclusion from 300-400 micromol/L from 48 – 60 hours of age. Infants with asphyxia and weight loss >10% were excluded. Infants were also excluded if their parents did not speak Swedish or if
the physician felt they would not be able handle home phototherapy.
In both environments treatment was provided with a biliblanket or overhead blue lights 25 cm from the skin which the infant would lay on or be placed under. These infants did not have severe bilirubin levels so it appears they had only standard phototherapy. This makes sense as babies with higher risk would not be suitable for consideration of home phototherapy.
Several validated tools were used to determine such things as bonding, risk of depression and stress. The primary outcome was based on use of the Postpartum Bonding Questionnaire (PBQ). Higher scores indicate worse bonding. The sample size was calculated on results from previous studies showing a mean (SD) of 10.7 (8.5) in 250 newborns with 90% power to detect a three-point difference in mean PBQ-sum for mothers at the 5% significance level, with a pre-planned interim analysis after 125 inclusions.
Enrollment was slow and after the preplanned analysis it was decided to stop the study recruitment and see where the results landed.
The Findings
Both groups of infants were treated for a total of about 4 days with testing for bilirubin levels and treatment with phototherapy (about 18 hours of total treatment both groups). The results of the PBQ found a statistical difference in measures of bonding favouring the home phototherapy group as found in the table below at both discharge and 4 months.
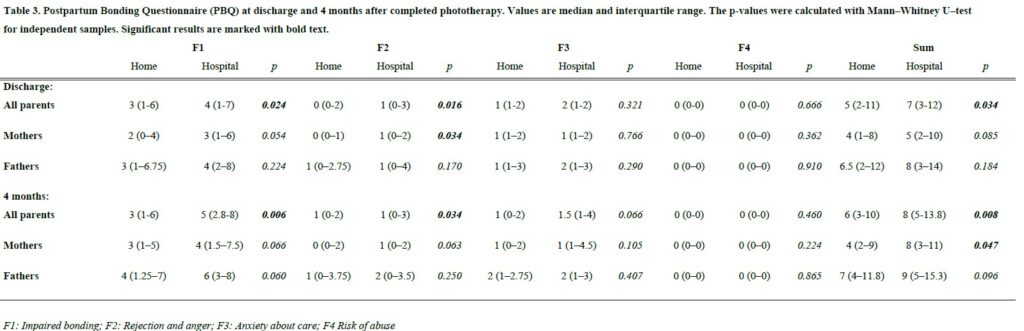
Interestingly when breaking down the results by mothers and fathers there was no impact on bonding for the fathers after this four day period of investigation and treatment at hospital vs in the home but at both time points it was the mother that drove the benefit seen. This likely speaks to differences in the way mothers and fathers experience bonding or perhaps how they process threats to it. No differences in stress could be found between the two groups but it is important to note that the small sample size and the fact that it was a secondary outcome make it difficult to say with certainty that there is no impact on stress.
Thoughts
You would be well within your rights to say “so what? It’s what we expected”. The difference seen in bonding while favouring the at home group has statistical significance but I am not sure to what degree this represents clinical significance. Can you truly perceive a difference in bonding based on a two point difference? Would that be meaningful functionally in the home in the way that parents relate to and respond to their infant? Not sure.
What I think we can say though is that the direction of the effect is certainly positive. We can also say from a systems standpoint that not only is phototherapy using a biliblanket safe and effective but it also moves care to the home and thereby creates room in the hospital for babies who truly need to be admitted.
Given the direction of the effect I think what the study does is provide one more argument aside from improving patient flow to aid in the establishment of home phototherapy programs. There are benefits not only to the family from an earlier discharge but also to some degree improvements in bonding certainly between mother and baby. This brief four day period has impacts that can last all the way out to four months. If you were looking for some evidence to support building such a program, maybe this will help!

