Non-sterile gloves to reduce NICU infections. Back to the Future?
I don’t know about you but I have deeply rooted memories from the 1990s of donning a yellow gown and gloves before examining each and every patient on my list before rounds. This was done as we firmly believed such precautions were needed to prevent the spread of infections in the NICU. As time went on though the gowns were removed and not long after so went the gloves as priority was placed on performance of good hand hygiene to reduce rates of infection in our units.
You can imagine that after having it entrenched in my mind that hand hygiene was the key to success that I would find it surprising to see a paper published a few months ago suggesting that the use of gloves after hand hygiene may offer a benefit after all. Kaufman DA et al published Nonsterile glove use in addition to hand hygiene to prevent late-onset infection in preterm infants: randomized clinical trial and given it’s challenge to a practice that is at least two decades old I thought it may be worth sharing with you the reader.
Essentially the authors hypothesized that the use of non-sterile gloves after performing hand hygiene (compared to hand hygiene alone) would reduce late-onset invasive infection (>72 hours after birth), defined as 1 or more episodes per patient of a BSI, urinary tract infection,meningitis, and/orNEC associated with clinical signs and symptoms of infection and treated with antimicrobials. When determining the size of study needed, they used a baseline incidence of 60% and looked to find a 25% reduction in their outcome. Unfortunately for them (although very fortunate for their patients, the incidence of LOS in the experimental arm was 32% with a 45% incidence in the control group (hand hygiene alone). What does this mean when your expected rate is higher than your observed? In short you need more patients to show a difference and indeed they failed to show a significant difference between the two groups. They did however find a difference in gram positive infections being 15 vs 32% p=0.03 and seem to take some comfort in this finding. If you were to give the paper a quick read you might be impressed with the finding and might even shrug your shoulders and say the common expression “Can’t hurt but might help” Maybe we should adopt this?
Not so Fast
There is a significant potential source of error here that needs to be addressed. The definition of a proven blood stream infection as per the CDC is two positive cultures for the same organism. In this study only one culture was required to be positive so the potential for diagnostic error is high. In our own centre although unpublished we have noted since adopting a mandatory two culture collection approach for LOS that there have been a significant number of occasions where one culture was noted to be positive and the other negative. Antibiotics in these cases have been stopped (for gram positive organisms) after 48 hours without consequence. In this study however the findings of increased rates of positive cultures in the hand hygiene only group is heavily influenced by the presence of only one positive culture as is seen in this table.
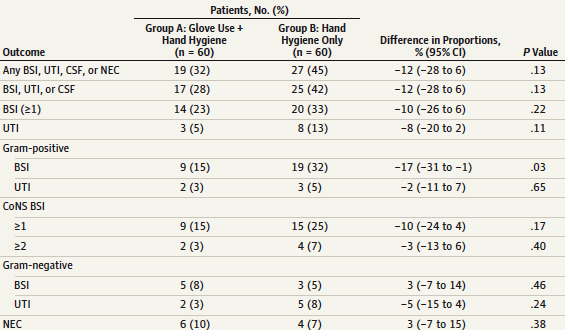
When looking at the numbers of times there were greater than or equal to 2 positive cultures in the CoNS group one sees the vast majority were only based on one culture. Furthermore, of the 20 infections in the hand hygiene only group, 19 were gram positve CoNS of which only 4 had more than one culture. Based on this finding and the lack of any other significant difference in infectious outcomes the proof that gloves add anything to reducing infection rates is tough to argue.
Could Gloves Actually Make Things Worse?
Several studies have actually indicated that wearing gloves reduces hand hygiene compliance. One such study although in adults “The dirty hand in the latex glove”: a study of hand hygiene compliance when gloves are worn. suggests that this is indeed the case with a 9% decrease in proper hand hygiene when gloves were worn. Others such as Flores in 2006 found similar poor perfomance when gloves were used Healthcare workers’ compliance with glove use and the effect of glove use on hand hygiene. I would speculate that although we all want to do what is best for our patients there may be a psychological trick being played here. Perhaps knowing we will cover up with gloves leads people to take shortcuts on hand hygiene as they subconciously think they will be covered anyway. Never mind that the “dirty” hand touches the gloves they will put on making proper hand hygiene a must.
Conclusion
It certainly was a shock to see such a paper as I saw flashes of my past yellow gowned self coming back to haunt me. Based on my take of this paper however I would say that at least for the time being I will take my time, wash my hands before and after every patient encounter and keep the gloves around for handling those yet unbathed newborns. Spend your energy where it counts and that is ensuring your hands are properly cleaned before touching your patient or lines.