Single Patient Room NICUs: Time to Put Parents Minds At Ease
Some time ago Nick Hall from Graham’s Foundation posted the following question on Linkedin:
Private room vs open bay for the NICU. Can always get a quote from a parent saying it is great but….? At what cost? Impact on staff? Is parent time in those NICUs greater now? Other alternatives?
Included in the post was an article discussing the benefits of such a design. Below I will look at the benefits and risks and conclude with an answer to his last question.
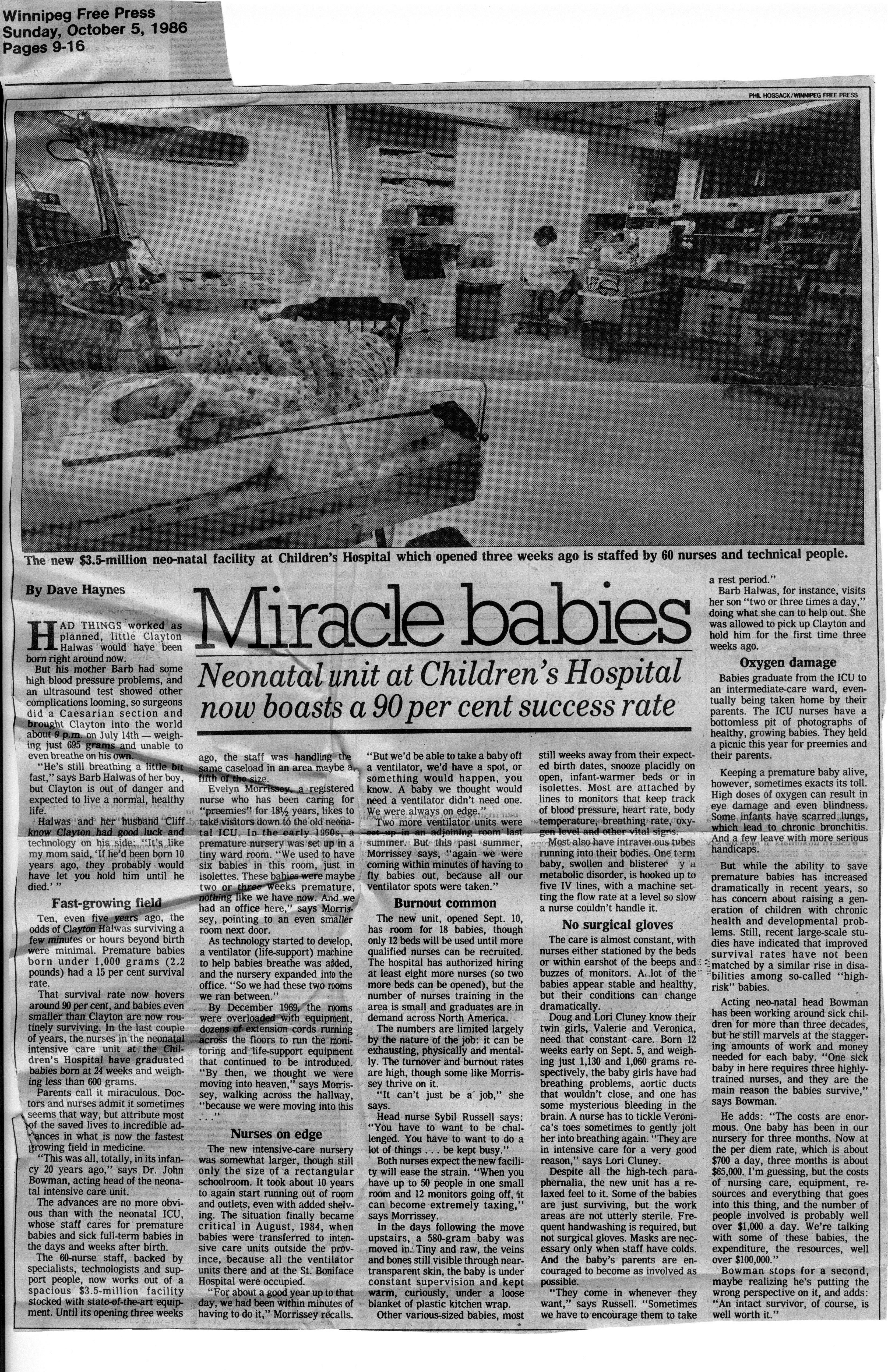
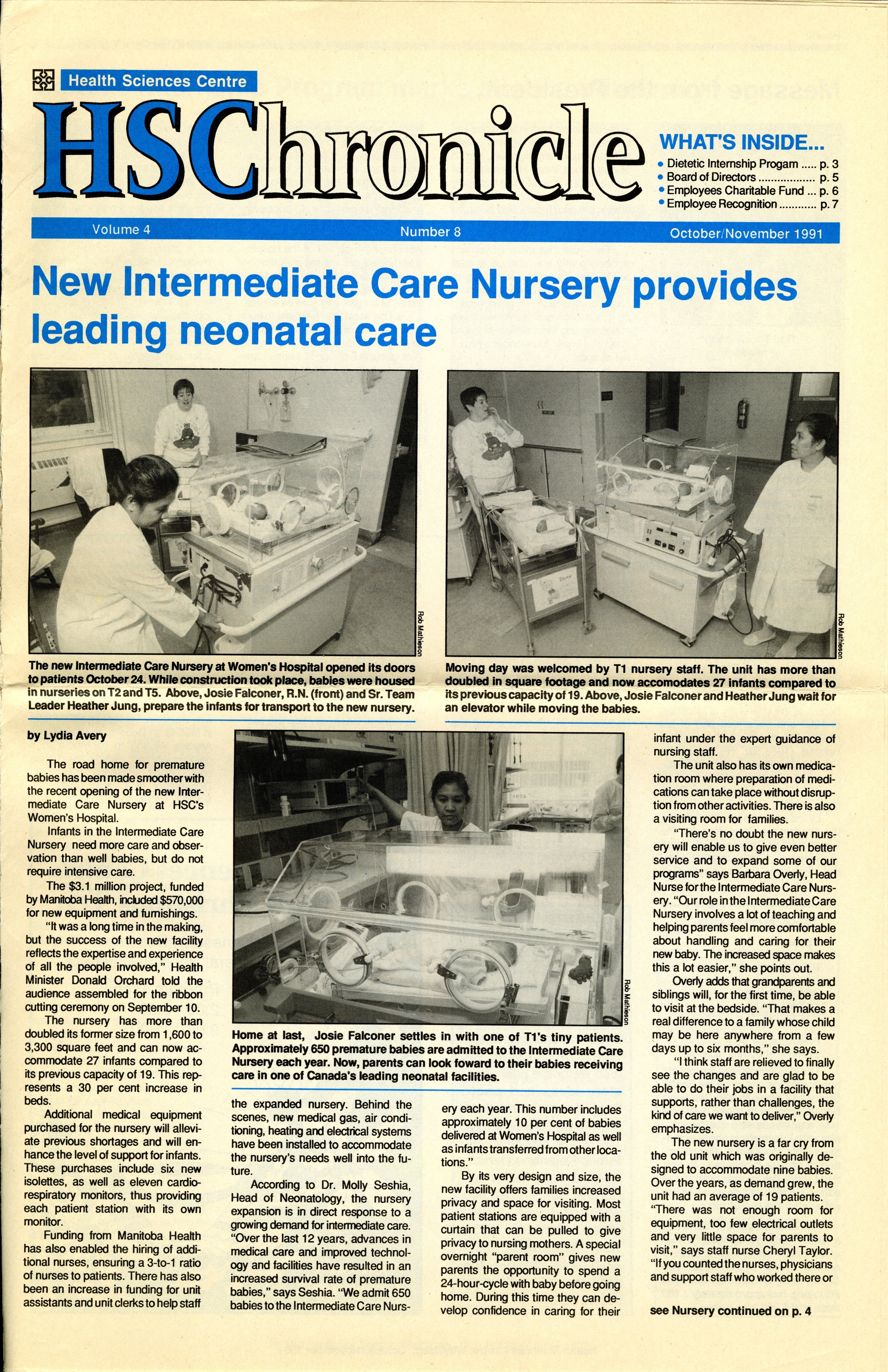
The NICUs of the 1970s through late 1990s have been described as “barn like” or “open concept” but in recent years the belief that single patient rooms (SPR) would offer greater benefit to infants led to the adoption of such a unit design across North America. The imagined benefits would be related to improved parent comfort, creating a desire for families to spend more time with their children. As we move to a “family centred” approach to care, a key goal of all units should be to make their families as comfortable and stress free as possible in order to have a positive experience.
Detractors meanwhile, speak of concern regarding isolation of such infants when families do not visit and moreover a risk that such infants deprived of sensory experience will have impaired development. Last year a paper was published that did not help quell such fears; Alterations in Brain Structure and Neurodevelopmental Outcome in Preterm Infants Hospitalized in Different Neonatal Intensive Care Unit Environments (full article in link). This study which compared infants cared for in SPR to an open unit (the hospital in this study had a mixture of both in their NICU) found a worrisome finding at 2 year follow-up in that the infants in SPR had lower scores on language and a trend towards lower motor scores as well. Additionally, partly explaining such findings may have been differences noted at term equivalent age in both the structure and activity of the children’s brains compared to those cared for in an open environment. We were starting construction on a new NICU at the time this paper was published and I can tell you the findings sent shockwaves through our hospital as many wondered whether this was the right decision.
Devil Is in The Details
Looking further into this study, the urban population bore little resemblance to our own. In our hospital all women are taught how to perform skin to skin care and the majority of our mothers spend a great deal of time with their infants. To see how successful have a look at our recent Kangaroo Care drive results! The families in this study however the average hours per week of parent visitation over the length of stay ranged from 1.8-104 hours with a mean of 19+/- 19 hours. The average number of days held per week over the length of stay was 0-6 days with a mean of 2.4 +/-1.5 days. The average number of days held skin-to-skin over the length of stay ranged from 0-4 days, with a mean of 0.7 +/- 0.9 days. In short they were hardly there.
Second Study Finds The Opposite
Later on in 2014 a second study on this subject was published; Single-family room care and neurobehavioral and medical outcomes in preterm infants. Infants < 1500g who were admitted to an NICU between 2008 and 2012 were compared with respect to medical and neurobehavioral outcomes at discharge. Participants included 151 infants in an open-bay NICU and 252 infants after transition to a SPR NICU.
Statistically significant results (all Ps ≤.05) showed that infants in the SPR NICU weighed more at discharge, had a greater rate of weight gain, required fewer medical procedures, had a lower gestational age at full enteral feed and less sepsis, showed better attention, less physiologic stress, less hypertonicity, less lethargy, and less pain. Nurses reported a more positive work environment and attitudes in the SPR NICU.
This study in fact demonstrated greater maternal involvement in a SPR with improvement in outcomes across the board. It would seem then that in a SPR environment, provided there is enough family visitation and involvement this model truly is superior to the open concept. Furthermore despite concerns by some nurses that the loss of line of sight to their patients will make for a more stressful working environment this does not seem to be the case.
What About Families Who Cannot or Simply Aren’t Visiting Frequently?
The reality is that there are many reasons for parents to be absent for long periods during their newborns stay. Having a home outside of the city with other children to care for, work obligations, or loss of custody and abandonment due to apprehension are just some of these reasons. In our hospital, at least 15-20% of all patients admitted are from outside Winnipeg. The evidence as I see it supports the move to a SPR but what do we do for those children who need more visitation? The solution is a cuddler program.
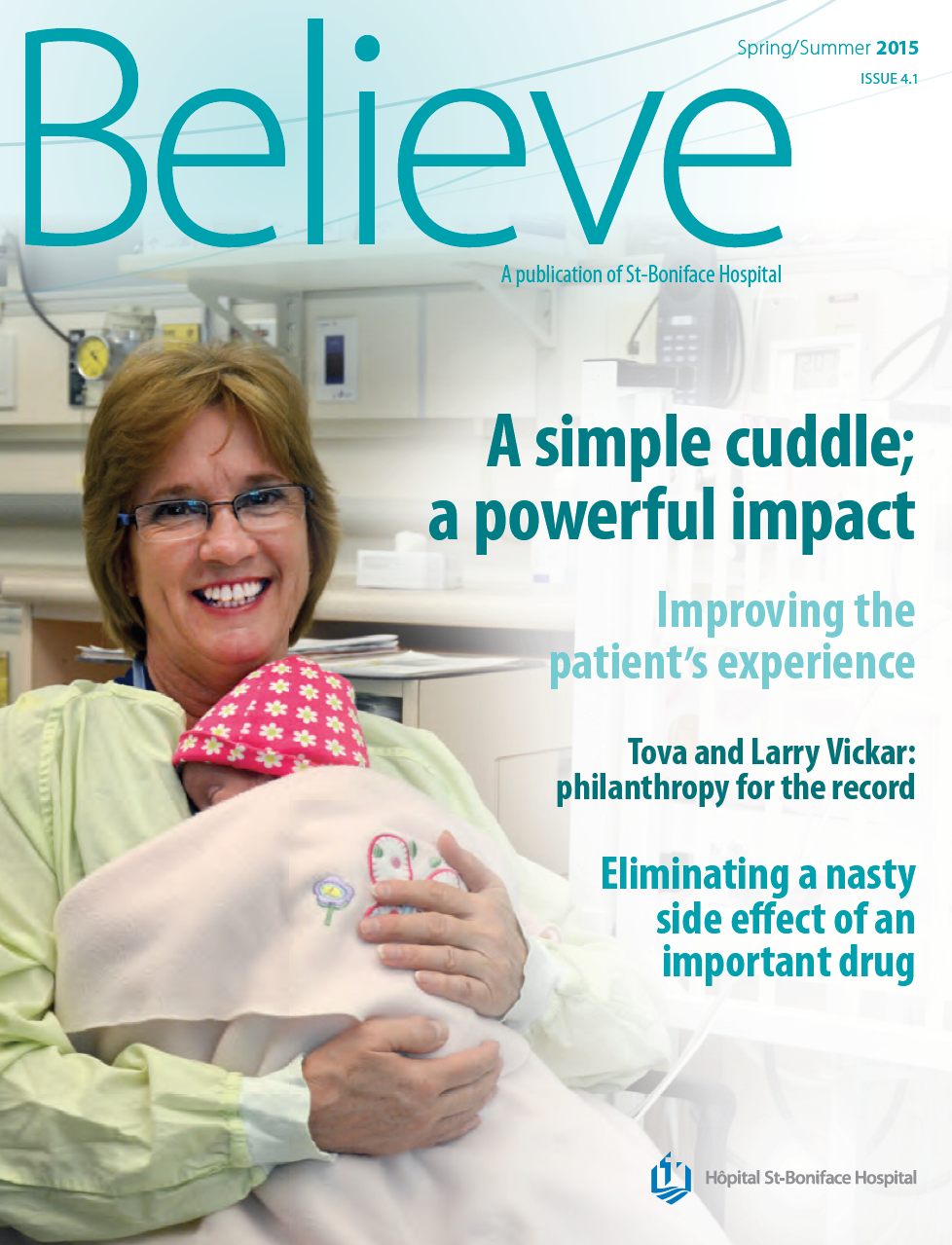 In our new hospital we are grateful for the generosity of our Children’s Hospital Foundation who secured a donor to pay for a coordinator of such a program. The veteran parent who is leading this program ensures that no infant goes beyond a set period of time without feeling the touch or hearing the sound of a voice. Such a program is in fact already in place at our other tertiary hospital and was featured in a lovely article attached here. Taking all the information together that is out there I think that if we can provide the necessary stimulation from both touch and auditory stimuli as well we can provide these infants with the developmental needs that each of them requires.
In our new hospital we are grateful for the generosity of our Children’s Hospital Foundation who secured a donor to pay for a coordinator of such a program. The veteran parent who is leading this program ensures that no infant goes beyond a set period of time without feeling the touch or hearing the sound of a voice. Such a program is in fact already in place at our other tertiary hospital and was featured in a lovely article attached here. Taking all the information together that is out there I think that if we can provide the necessary stimulation from both touch and auditory stimuli as well we can provide these infants with the developmental needs that each of them requires.
The SPR is the right design in my mind for families with many benefits that spring forth in such an environment. This need not be a win-lose scenario for your hospital. Do not underestimate the power of a cuddler and don’t hesitate to seek support to initiate such a program. It could mean the difference from going from good to great!
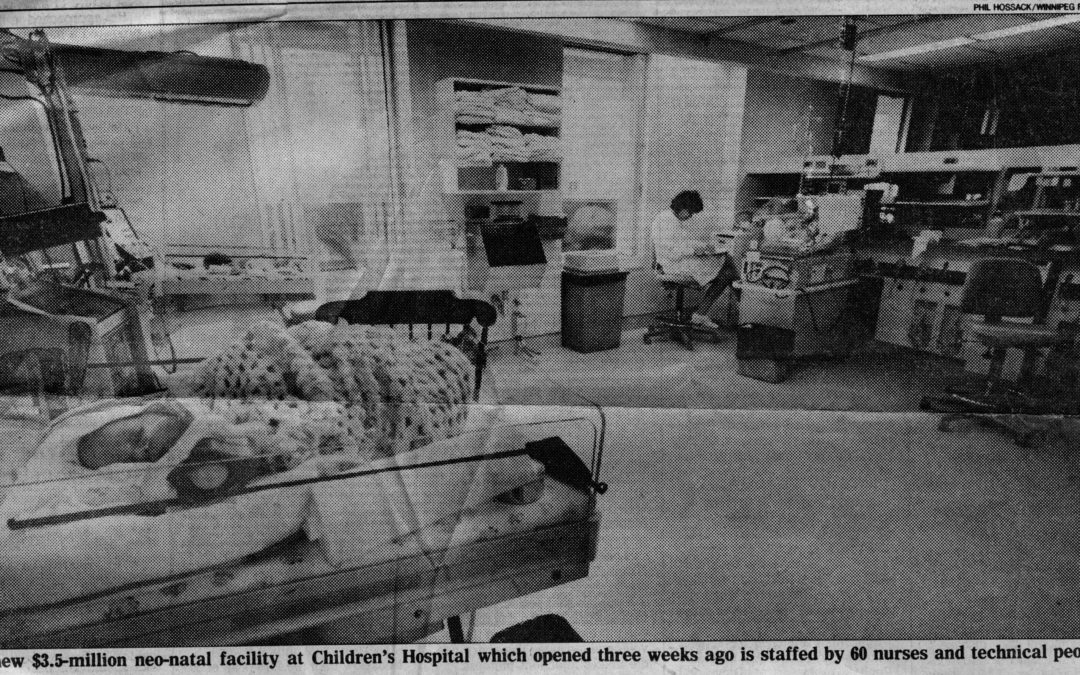
 If your unit is anything like ours where you work I imagine you feel as if you are bursting at the seams. As the population grows so do our patient volumes. I often quote the number 10% as being the number of patients we see out of all deliveries each year in our units. When I am asked why our numbers are so high I counter that the answer is simple. For every extra 100 births we get 10 admissions. It is easy though to get lost in the chaos of managing a unit in such busy times and not take a moment to look back and see how far we have come. What did life look like 30 years ago or 25 years ago? In Winnipeg, we are preparing to make a big move into a beautiful new facility in 2018. This will see us unify three units into one which is no easy task but will mean a capacity of 60 beds compared to the 55 operational beds we have at the moment.
If your unit is anything like ours where you work I imagine you feel as if you are bursting at the seams. As the population grows so do our patient volumes. I often quote the number 10% as being the number of patients we see out of all deliveries each year in our units. When I am asked why our numbers are so high I counter that the answer is simple. For every extra 100 births we get 10 admissions. It is easy though to get lost in the chaos of managing a unit in such busy times and not take a moment to look back and see how far we have come. What did life look like 30 years ago or 25 years ago? In Winnipeg, we are preparing to make a big move into a beautiful new facility in 2018. This will see us unify three units into one which is no easy task but will mean a capacity of 60 beds compared to the 55 operational beds we have at the moment.