Inhaled nitric oxide has been around for some time now. I recall it being called at one point in medical school “endothelial relaxation factor” and then later on identified as nitric oxide. Many years later it finds itself in common usage in NICUs all over the world. Our experience though has been for treatment of pulmonary hypertension and for that it is pretty clear that for those afflicted by that condition it can be lifesaving. Over the years other uses have been looked at including prevention of BPD (turned out not to be the case). Rescue approaches therefore have found to be useful but on the prophylactic side of things not so much.
Maybe starting earlier is the key?
A group based out of Oklahoma has published a pilot study that raised an eyebrow for me at least. Krishnamurthy et al released Inhaled Nitric Oxide as an Adjunct to Neonatal Resuscitation in Premature Infants: A pilot, double blind, randomized controlled trial . The study set out to recruit 40 infants who between 30-90 seconds of life if requiring PPV would either get iNO 20 ppm with 30% oxygen or 30% oxygen and placebo for ten minutes. At ten minutes weaning of iNO by 1 ppm per minute for a total of 17 minutes was done. The primary outcome of interest was FiO2 required to achieve target oxygen saturations. As with many studies that seek enrollment prior to delivery this study was a challenge as well with early termination of the study after 28 babies (14 in each group) were recruited.
Did they find anything interesting?
In spite of the low numbers in the study, the authors did find a divergence in the FiO2 needed to achieve the target oxygen saturations.
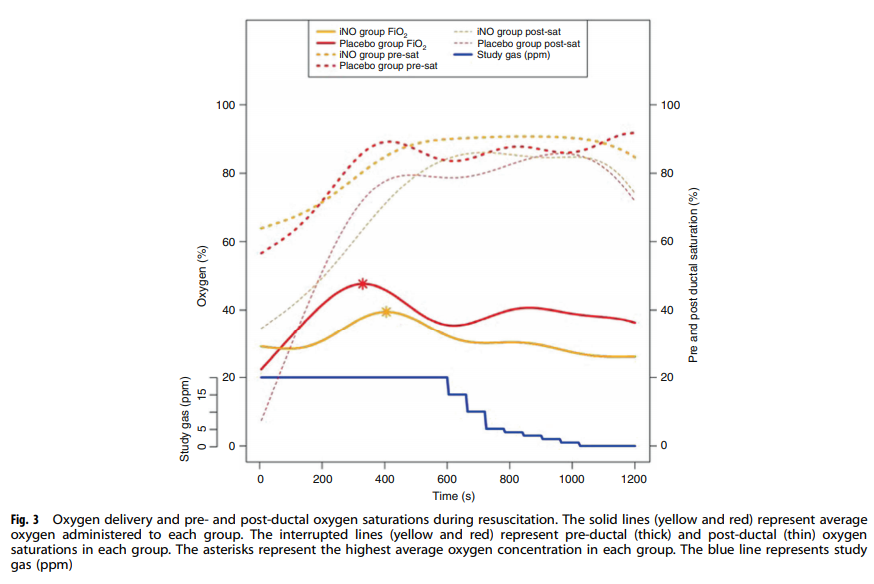
The authors conclusions were that the cumulative exposure to FiO2 was lower in the iNO group as well as the maximum exposed FiO2 of 39% vs 48% (although this almost but not quite met statistical significance. Even then this is a pilot study so inferring too much could be a dangerous thing.
The study though does get one thinking but we need to be wary of letting our brains do some mental trickery. Lower FiO2 seems like a good thing given what we know about oxygen free radicals. What about rapid lowering of pulmonary vascular resistance with exogenous iNO? Is this a good thing or could other things be lurking around the corner? Could a larger study for example find a higher rate of pulmonary hemorrhage with rapid reductions in PVR? The authors did not find harm in the study but again with small numbers it is hard to conclude too much.
What this small study does though is raise many questions that I think could be interesting to answer. If a patient needs less FiO2 at 17 minutes after study entry might there be less perceived need for higher PEEP if ventilated or CPAP levels if on non-invasive support? Less pressure could lead to less risk of pneumothorax (or more perhaps if under treated but with respiratory distress. Less pressure might also influence longer term risks of BPD from barotrauma or volutrauma for that matter.
Regardless this is only the beginning. I have no doubt there will be further trials on the way. The trick will be as in this study to obtain consent unless a deferred consent could be obtained but I have my doubts about getting that. Nonetheless, wait for more to come!

Pulmonary pressures coming down to soon would augment the haemodynamic changes ( maximum being in first 24 hours) of PDA by causing increased left to right shunt in first few minutes of life when we are are trying to increase systemic flow. More important is to increase FRC so that pulmonary capillaries open up and establish proper ventilation perfusion ratios. Decreasing pulmonary pressures by iNO too soon may not be too good an idea