In the book Outliers by Malcolm Gladwell he talked about 10000 hours being the threshold at which if you practiced or gained that much experience with something you could become an expert. In Sweden the approach to 22 week pregnancies and above is to resuscitate all as a strategy. I wrote about this before in At 22 weeks of gestation does your faith matter most to outcome? The information gleaned from that paper was that if you have a policy of resuscitation at these gestational ages and you compare outcomes to a centre that is selective in who they resuscitate the outcomes are better when you believe all should be resuscitated.
New Study Expands Data
The same group has published this time around the results of the same cohort from 2006-2015 but this time with developmental outcome data. The paper is entitled Outcomes of a uniformly active approach to infants born at 22-24 weeks of gestation In this paper they discuss outcomes at 234 and 24 weeks respectively in addition to the findings for 22 weeks which they covered in the paper mentioned above. The reason for sharing this study is that if I asked you to imagine going into a room right now and talking to a family at 22 – 24 weeks and predicting the outcome of their infant, my hunch is that you would not provide as rosy a picture as the group in Uppsala, Sweden.
The authors looked at a group of infants with the following breakdown by gestational age.
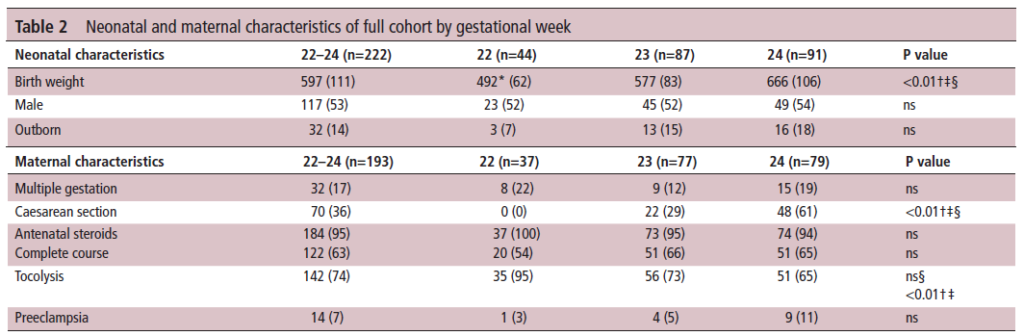
As you can see, there were 222 infants in total and reasonable samples at each gestational age. What differs from other larger reports such as the work by Rysavy et al in Between-Hospital Variation in Treatment and Outcomes in Extremely Preterm Infants is that in this study ALL infants were resuscitated with intention.
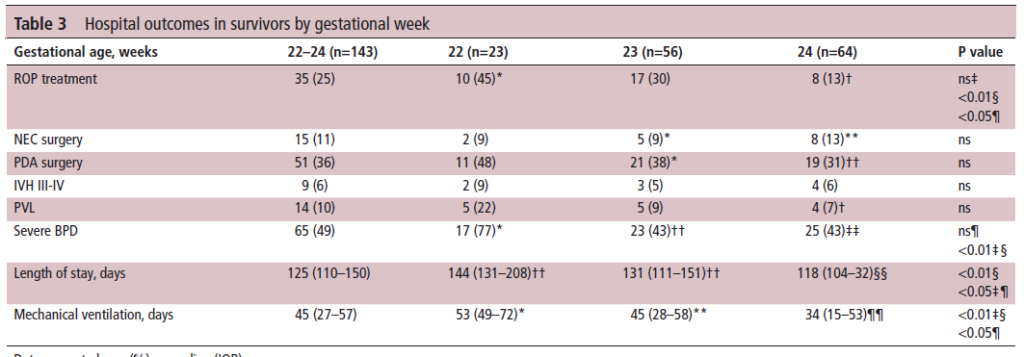
Not surprisingly as gestational age declines the incidence of complications rise but looking at Table 3 even at 22 weeks there was no difference in rate of NEC or need for PDA surgery. Nor was there a difference in rates of severe IVH/PVL. Rates of BPD were higher and likely attributable to the longer durations of positive pressure ventilation. Are these rates for these complications terrible though when the other option is non-intervention which for certain means death?
What about outcome?
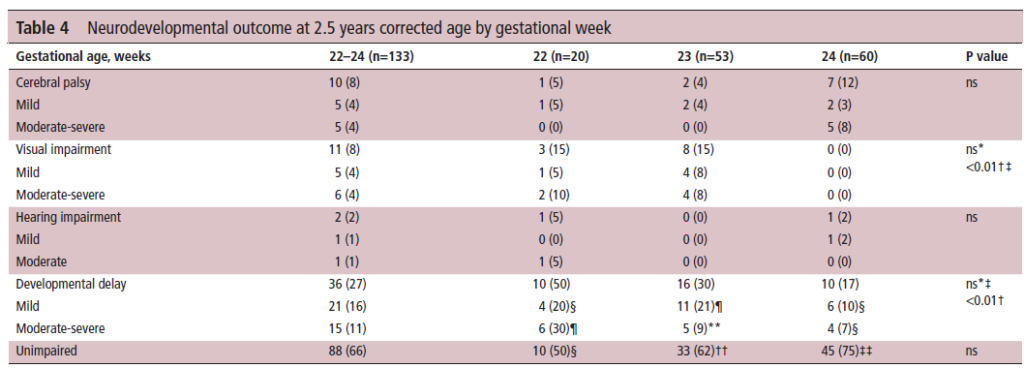
Looking at the outcome at 2.5 years, the rate of cerebral palsy is about 1:10 to 1:20 for all GA. Hearing impairment is almost non-existent and while developmental delay is detected in 50 percent of survivors at 22 weeks only about a quarter of the infants have severe impairment.
Deciding what to do
There is no question that many of you seeing what this post was about would simply say “NO WAY” but in the end isn’t it really about a shared decision with the family? It wasn’t that long ago that we had to have a real paradigm shift in thinking about resuscitating 23 week infants. The amount of mental energy spent for teams worldwide coming to this decision was tremendous and now if you were to suggest compassionate care at 24 weeks you get a look back like you are crazy! It wasn’t that long ago that 24 weeks was considered viability in many places and now that 23 is the new 24 this is the struggle some people have now. Should we go to 22 weeks everywhere as the Swedes have? Clearly this is a decision that institutions need to look at critically and determine if they have the space to accomodate. Each infant should they survive will occupy a bed for at least 6 months. This needs to be looked at before one can just say sure this is a good idea.
In the end what the study demonstrates I believe is that the outcome at 22 and 23 weeks for that matter need not be universally dismal. There certainly is a good chance that a surviving infant will have one or more deficits but in the end I would advocate this is a conversation all units need to be having and critically look at whether each institution has the capactity to consider.
My bet is that five years from now this discussion will be moot as we will be mostly in that direction but at this time I think we are still in evolution.