If you work in Neonatology or in Pediatrics for that matter there is no doubt that at some point you took the neonatal resuscitation program (NRP). Ideally you should be recertified every year or two years depending on your profession. In the course you are taught that the depth of chest compressions required to achieve the best chances of ROSC is 1/3 the diameter of the chest. The evidence to support this comes from a CT evaluation of neonatal thoraces in the paper Evaluation of the neonatal resuscitation program’s recommended chest compression depth using computerized tomography imaging. In this study the authors found that using a mathematic model the 1/3 chest compression recommendation should in theory yield the best hemodynamic outcome.
What about ROSC?
Hemodynamics is one thing in a model but what about real life? I don’t think you could reasonably do an RCT these days with the outcome of interest being ROSC in humans. What research ethics board would allow you to randomize to the outcome of death in babies and deviate from an international organizations recommendations for best practice? My former colleagues in Edmonton had an answer to this issue though by using a piglet model to test the hypothesis that 33% is indeed better than either 12.5%, 24% or 40% chest compression depth. Their paper Assessment of optimal chest compression depth during neonatal cardiopulmonary resuscitation: a randomised controlled animal trial tackles just that question.
How did they do it? In an animal lab that is equipped with a mechanical device to simulate chest compressions they were able to instrument piglets and after asphyxiating them with an occluded ETT they began the process of trying to revive them. After being asphyxiated they initiated a combination of PPV with a neopuff and gave epinephrine (0.02 mg/kg/dose) intravenously2 min after the start of positive pressure ventilation and every 3 min until ROSC with a maximum of three doses, with a maximum resuscitation time of 10 min. The groups were divided in the following manner.

What did they find?
Two very interesting things came out of the study. The first was that they abandoned the 12.5% group early in the study when it became apparent that no piglet would survive using this depth. The other thing they found in support of greater depths of 33 and 40% compression depth is shown in the following graph.
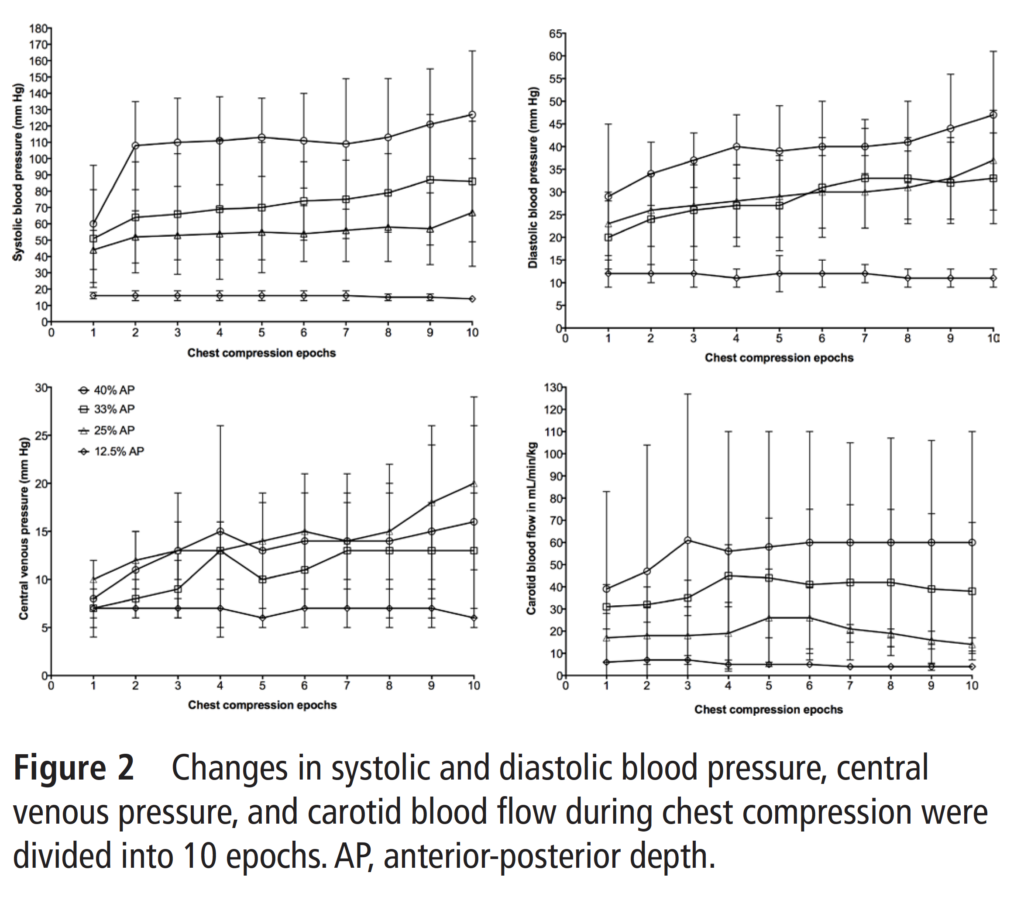
The authors found that in terms of systolic and diastolic blood pressure the best chances in particular for systolic blood pressure were the 33 and 40% compression depths. Looking at the bottom right figure it is also evident that cerebral blood flow increases with increasing depth of compression.
With respect to the primary outcome they found this:
“The median (IQR) time to ROSC was 600 (600–600) s, 135 (90–589) s, 85 (71–158)* s and 116 (63–173)* s for the 12.5%, 25%, 33% and 40% AP depth groups, respectively (p<0.001 vs 12.5% AP depth group). The number of piglets that achieved ROSC was 0 (0%), 6 (75%), 7 (88%)** and 7 (88%)** in the 12.5%, 25%, 33% and 40% AP depth groups, respectively (*p<0.05 and **p<0.005 vs 12.5% AP depth group).
Of note, one of the piglets randomized to 40% depth of compression had pulmonary contusions at autopsy.
Putting it all together
The article supports the use of 33-40% chest compression but it raises an important point in my mind. The study used a mechanical device to ensure the percentage compression and it is clear that if you fall below these numbers the ROSC and hemodynamics is impaired while if you go to high you run the risk of damaging the lungs (I know it was just one but a previous study demonstrated harm at 50% compression depth as well).
This raises the question about failed resuscitations. Do we know how deep we are actually compressing during these situations? Sure, everyone can recite that we should be compressing to 1/3 of the chest diameter but what are we actually doing? In some cases are we not doing enough and in other cases doing way to much? I would imagine the answer to this question is yes. I do wonder as we continue to automate so much in our world through advances in technology if doing the same in neonatal resuscitation is not that far off. When our hands are sweaty and tremulous with adrenaline coursing through our veins how good are we really at controlling the precise depth of compression. Time will tell what happens but what is clear to me is that precision matters and really how precise can we be?

I’m gonna add to the questions….
In Micropremie’s less than (I dunno..) 24 weeks-ish?….should we be doing chest compressions OR are we just bruising their lungs to the point of not being functional, liberating all that potassium and just making them worse?
There. I said it out loud.